Group B Streptococcus (GBS) is a common bacterial pathogen that can cause severe infections in different parts of the body. While it is best known for causing neonatal infections, GBS has also been implicated in pelvic inflammatory disease (PID), a serious infection affecting the female reproductive organs. Understanding the connection between GBS and PID is crucial for effective prevention, diagnosis, and treatment.
What is Group B Streptococcus (GBS)?
Group B Streptococcus (Streptococcus agalactiae) is a Gram-positive bacterium commonly found in the gastrointestinal and genitourinary tracts. Although it is generally asymptomatic in healthy individuals, GBS can become opportunistic and cause invasive infections under certain conditions.
Key Characteristics of GBS:
- Gram-positive coccus bacterium
- Colonizes the gastrointestinal and vaginal tracts
- Leading cause of neonatal sepsis and meningitis
- Capable of causing urinary tract infections, pneumonia, and bacteremia in adults
Understanding Pelvic Inflammatory Disease (PID)
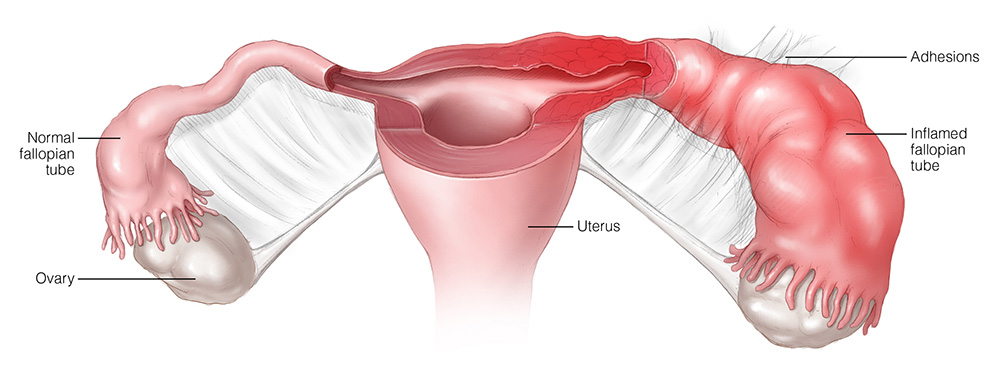
Pelvic Inflammatory Disease (PID) is an infection of the female reproductive organs, including the uterus, fallopian tubes, and ovaries. PID is typically caused by sexually transmitted bacteria such as Neisseria gonorrhoeae or Chlamydia trachomatis, but GBS can also contribute to this condition.
Risk Factors for PID:
- Multiple sexual partners
- Unprotected sexual activity
- Prior history of sexually transmitted infections (STIs)
- Douching, which disrupts the vaginal microbiome
The Link Between GBS and PID
Although GBS is not a primary cause of PID, studies have shown that it can contribute to pelvic infections, particularly in postpartum or post-surgical patients. GBS-related PID may present differently than traditional PID cases, often showing more severe systemic symptoms.
How GBS Contributes to PID:
- Postpartum Endometritis: GBS is a notable cause of postpartum infections that can progress to PID.
- Post-Surgical Infections: Women undergoing gynecological procedures are at increased risk for GBS-induced PID.
- Immune Compromise: Patients with weakened immune systems are more vulnerable to GBS-related PID complications.
Symptoms of GBS-Associated PID
The symptoms of PID caused by GBS are often similar to those caused by other pathogens but may be more severe.
Common Symptoms:
- Severe lower abdominal pain
- Abnormal vaginal discharge with an unpleasant odor
- Fever and chills
- Pain during intercourse or urination
- Irregular menstrual bleeding
Diagnosis of GBS-Related PID
Accurate diagnosis is essential for prompt treatment. Physicians typically employ several methods to identify GBS and confirm PID.
Diagnostic Techniques:
- Pelvic Examination: Identifies tenderness, cervical motion pain, and abnormal discharge
- Culture Tests: Vaginal and cervical swabs to detect GBS presence
- Ultrasound Imaging: Helps visualize abscesses or inflamed fallopian tubes
- Blood Tests: Indicate elevated white blood cell counts and inflammatory markers
Treatment Options for GBS-Related PID
Effective management requires targeted antibiotics and supportive care to prevent complications such as infertility or chronic pelvic pain.
Recommended Treatment Protocols:
- Antibiotic Therapy: Penicillin and cephalosporins are first-line treatments for GBS infections.
- Hospitalization: Severe cases with systemic involvement may require intravenous antibiotics and close monitoring.
- Pain Management: Non-steroidal anti-inflammatory drugs (NSAIDs) are often prescribed to reduce discomfort.
- Partner Treatment: Sexual partners may need evaluation and treatment to prevent reinfection.
Preventing GBS-Associated PID
Preventive strategies are crucial to reducing the risk of GBS-related PID.
Key Prevention Measures:
- Routine screening for GBS during pregnancy
- Practicing safe sex and consistent condom use
- Avoiding vaginal douching
- Prompt treatment of vaginal or urinary tract infections
Potential Complications
If left untreated, GBS-related PID can lead to severe complications such as:
- Ectopic pregnancy
- Infertility
- Chronic pelvic pain
- Abscess formation in the reproductive organs
Group B Streptococcus, while traditionally associated with neonatal infections, is an emerging contributor to pelvic inflammatory disease in certain populations. Early diagnosis, prompt treatment, and preventive measures are key to managing GBS-related PID effectively. By improving awareness and adopting preventive strategies, we can reduce the incidence and complications of this serious condition.
FAQs
Is GBS a common cause of PID?
GBS is not a primary cause of PID, but it can contribute to PID in postpartum or post-surgical patients.
How is GBS diagnosed in PID cases?
GBS diagnosis typically involves culture testing from vaginal or cervical swabs, along with clinical assessment.
Can GBS-induced PID be prevented?
Routine GBS screening during pregnancy, safe sex practices, and proper hygiene can reduce the risk of GBS-related PID.
What antibiotics are effective for GBS-related PID?
Penicillin, ampicillin, and cephalosporins are commonly prescribed for GBS infections.
What are the risks if GBS-related PID is untreated?
Untreated cases may lead to infertility, chronic pain, and life-threatening abscesses.