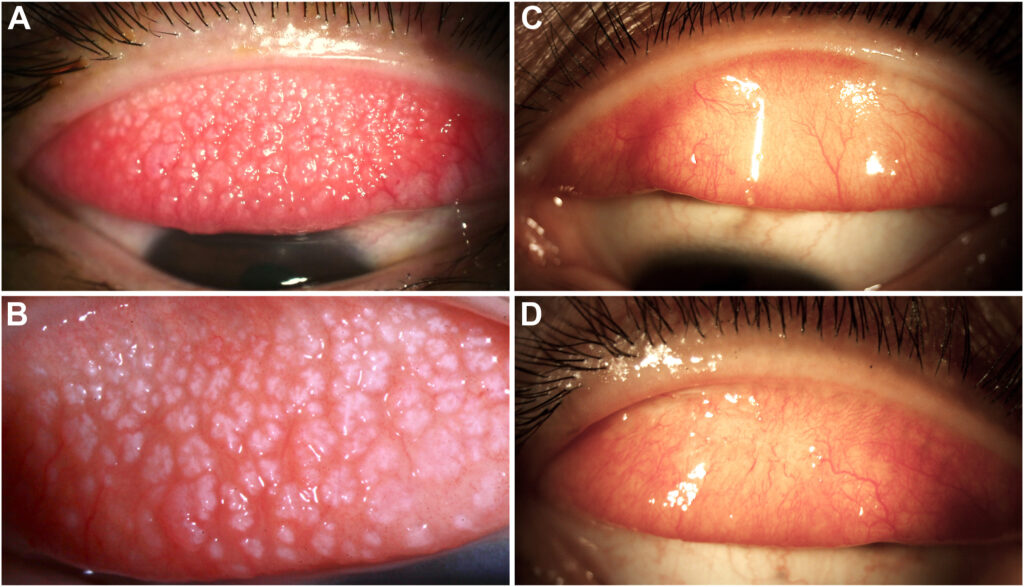
Giant papillary conjunctivitis (GPC) is a chronic inflammatory condition affecting the inner surface of the eyelid. It commonly occurs in individuals who wear contact lenses or have ocular prosthetics. Characterized by enlarged papillae on the upper eyelid’s inner surface, GPC can cause significant discomfort and visual disturbances if left untreated.
Causes of Giant Papillary Conjunctivitis
Several factors can contribute to the development of GPC:
- Contact Lenses: Prolonged use of soft lenses, particularly extended-wear or poorly maintained lenses.
- Ocular Prosthetics: Artificial eyes or intraocular implants may trigger irritation.
- Sutures or Surgical Residues: Post-operative materials can lead to GPC.
- Allergic Reactions: Certain allergens can exacerbate the condition.
Symptoms of Giant Papillary Conjunctivitis
The symptoms of GPC typically develop gradually and may include:
- Persistent itching and irritation
- Redness in the inner eyelid
- Mucus discharge, particularly upon waking
- Foreign body sensation in the eye
- Blurry vision due to excess mucus or lens movement
- Papillae formation on the inner eyelid (visible in severe cases)
Risk Factors for Giant Papillary Conjunctivitis
Certain individuals are more prone to developing GPC:
- Contact Lens Wearers: Especially those using soft lenses or wearing lenses overnight.
- Post-Operative Patients: Individuals with corneal sutures or implants.
- Allergy Sufferers: Seasonal or environmental allergies can elevate the risk.
Diagnosis of Giant Papillary Conjunctivitis
A comprehensive eye examination is crucial for diagnosis. This may involve:
- Slit-Lamp Examination: To inspect the conjunctiva and assess papillae size.
- Medical History Review: Identifying risk factors like allergies or contact lens usage.
- Tear Film Analysis: To evaluate the eye’s lubrication and detect mucus buildup.
Treatment for Giant Papillary Conjunctivitis
1. Contact Lens Management
- Switch to daily disposable lenses to minimize protein deposits.
- Implement proper lens hygiene, including regular cleaning and disinfection.
- Reduce lens wear duration to give the eyes recovery time.
2. Pharmacological Treatment
- Antihistamine Eye Drops: To alleviate itching and inflammation.
- Mast Cell Stabilizers: Prevent the release of histamines that trigger allergic responses.
- Corticosteroid Eye Drops: For severe inflammation (under medical supervision).
3. Surgical Intervention
- In extreme cases, surgical removal of sutures or implants may be necessary.
- Excision of particularly large papillae may be advised in rare conditions.
4. Allergen Management
- Minimize exposure to known allergens.
- Use air purifiers and regularly clean bedding to reduce allergen accumulation.
Prevention of Giant Papillary Conjunctivitis
- Maintain proper contact lens hygiene and storage practices.
- Replace lenses regularly to prevent protein buildup.
- Use preservative-free artificial tears to reduce irritation.
- Avoid excessive eye rubbing to minimize mechanical irritation.
When to Seek Medical Attention
Prompt medical attention is crucial if you experience:
- Persistent eye discomfort despite lens hygiene improvements
- Significant vision disturbances
- Excessive mucus discharge or redness
Giant papillary conjunctivitis is a manageable condition when diagnosed early and treated effectively. Proper lens care, medication, and preventive measures can significantly reduce symptoms and improve overall eye health.
FAQs
Q1: Can GPC occur in non-contact lens wearers?
Yes, GPC can develop due to ocular prosthetics, post-surgical residues, or severe allergies.
Q2: Is GPC contagious?
No, GPC is an inflammatory condition and not an infectious disease.
Q3: Can I continue wearing contact lenses if I have GPC?
Yes, but your doctor may recommend switching to daily disposable lenses or reducing usage.
Q4: Are there natural remedies for GPC?
Warm compresses and preservative-free artificial tears can provide some relief but should be used alongside medical treatment.
Q5: How long does GPC treatment take?
With proper treatment, symptoms often improve within a few weeks, though complete recovery may take longer for severe cases.