Chlamydia trachomatis is the most common bacterial sexually transmitted infection (STI) globally, often affecting the genitourinary tract. It frequently presents asymptomatically, leading to underdiagnosis and untreated cases, which can cause severe reproductive and urological complications.
Etiology and Pathophysiology
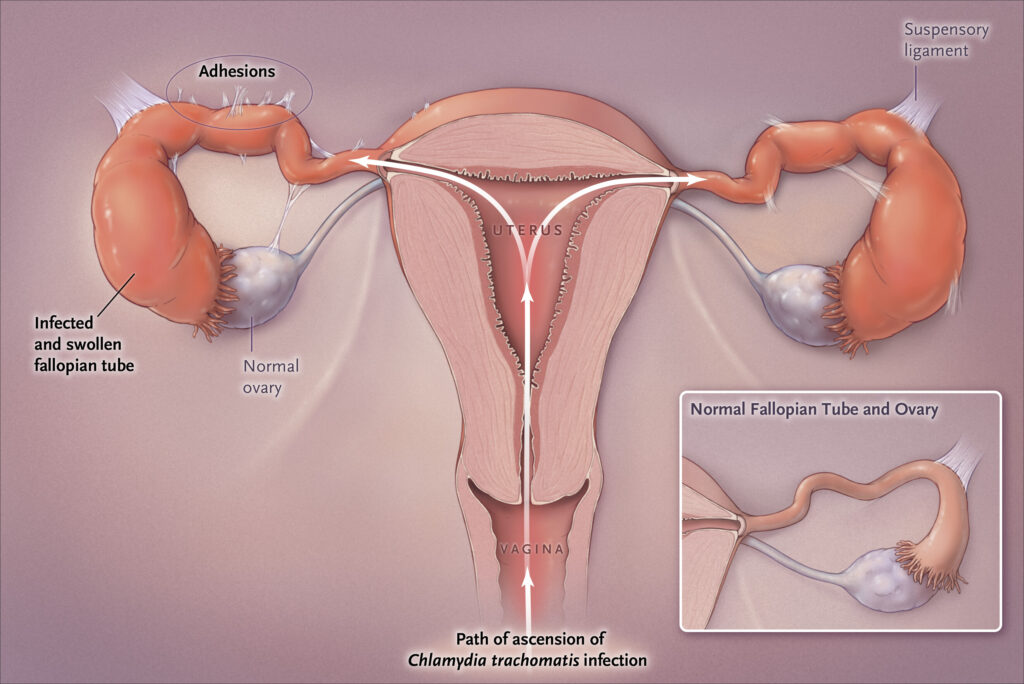
Chlamydia trachomatis is an obligate intracellular bacterium that infects epithelial cells of the urogenital tract. The infection triggers an inflammatory response, leading to urethritis, cervicitis, and potential upper reproductive tract involvement, such as pelvic inflammatory disease (PID) in women and epididymitis in men.
Modes of Transmission
- Unprotected vaginal, anal, or oral intercourse
- Vertical transmission from mother to child during childbirth
- Contaminated fingers transferring bacteria from genital areas to the eyes (causing trachoma)
Symptoms of Genitourinary Chlamydia Infection
In Males
- Urethritis (burning sensation during urination)
- Mucoid or watery penile discharge
- Testicular pain and swelling (epididymitis)
- Increased urinary frequency
In Females
- Cervicitis with mucopurulent discharge
- Dysuria and urinary urgency
- Post-coital bleeding
- Lower abdominal pain
- Dyspareunia (pain during intercourse)
Asymptomatic Cases
Over 70% of infected females and 50% of males remain asymptomatic, making routine screening crucial.
Complications of Untreated Chlamydia Infection
- In Women: Pelvic inflammatory disease (PID), infertility, ectopic pregnancy, chronic pelvic pain
- In Men: Epididymitis, prostatitis, infertility
- Neonatal Infection: Conjunctivitis, pneumonia in newborns
- Reactive Arthritis: Associated with the triad of arthritis, urethritis, and conjunctivitis (Reiter’s syndrome)
Diagnosis of Chlamydia trachomatis Infection
Laboratory Tests
- Nucleic Acid Amplification Test (NAAT): Gold standard for detection
- Urine Samples: First-catch urine specimen (preferred for men)
- Cervical/Vaginal Swabs: Preferred for female patients
- Rectal and Pharyngeal Swabs: For individuals engaging in receptive anal or oral sex
Differential Diagnosis
- Gonorrhea
- Mycoplasma genitalium infection
- Bacterial vaginosis
- Urethritis from non-STI causes (e.g., urinary tract infections)
Treatment and Management
First-Line Antibiotics
- Azithromycin (1g single dose, oral)
- Doxycycline (100 mg twice daily for 7 days)
Alternative Treatments
- Erythromycin, Levofloxacin, or Ofloxacin in case of contraindications
Partner Treatment and Follow-Up
- All recent sexual partners (past 60 days) should be tested and treated
- Abstinence from sexual activity until treatment completion
- Test-of-cure required for pregnant women and cases with persistent symptoms
Prevention Strategies
Behavioral Approaches
- Consistent condom use
- Regular STI screenings for sexually active individuals
- Reducing the number of sexual partners
Public Health Measures
- Educational campaigns promoting awareness
- Expedited partner therapy (EPT) programs
- Vaccination research efforts (ongoing but currently unavailable)
Frequently Asked Questions:
1. Can chlamydia go away on its own?
No, untreated chlamydia can persist for months and lead to complications. Antibiotic treatment is necessary.
2. How long does it take for chlamydia symptoms to appear?
Symptoms typically appear within 1-3 weeks of exposure but can take longer or remain asymptomatic.
3. Can I get reinfected with chlamydia after treatment?
Yes, reinfection is common. Regular testing and partner treatment are essential to prevent recurrence.
4. Is chlamydia only transmitted through penetrative sex?
No, it can also be transmitted through oral and anal sex, as well as perinatally from mother to child.
5. How often should I get tested for chlamydia?
Sexually active individuals under 25 and those with multiple partners should be screened annually.
Genitourinary Chlamydia trachomatis infection remains a significant public health concern due to its high prevalence and potential complications. Timely screening, accurate diagnosis, and appropriate treatment are crucial in managing and preventing its spread. Public awareness and safe sexual practices play a vital role in reducing transmission rates and associated morbidities.

