Genital organ pruritus, commonly referred to as genital itching, is a prevalent condition affecting individuals of all genders and ages. This discomfort can significantly impact one’s quality of life, making daily activities and intimate relationships challenging. Understanding the underlying causes, recognizing associated symptoms, and seeking appropriate treatment are crucial steps toward effective management and prevention.

Common Causes of Genital Pruritus
Several factors can lead to genital itching, ranging from infections to dermatological conditions. Below, we outline some of the most common causes:
1. Infections
- Fungal Infections (Yeast Infections): Overgrowth of Candida species can result in intense itching, redness, and a thick, white vaginal discharge.
- Bacterial Vaginosis: An imbalance in vaginal bacteria can cause itching accompanied by a thin, grayish discharge with a fishy odor.
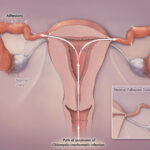
- Sexually Transmitted Infections (STIs): Conditions such as trichomoniasis, genital herpes, and human papillomavirus (HPV) infections can present with itching and other symptoms.
- Pubic Lice (Crabs): Infestation by pubic lice leads to itching and a sensation of crawling in the genital area.
2. Dermatological Conditions
- Lichen Sclerosus: A chronic condition causing thin, white patches on the genital skin, leading to itching and discomfort.
- Lichen Simplex Chronicus: Resulting from chronic scratching or rubbing, this condition leads to thickened, leathery skin in the affected area.
- Psoriasis: A chronic inflammatory condition that can affect the genital area, causing red, itchy patches.
- Contact Dermatitis: Exposure to irritants or allergens, such as soaps, detergents, or fabrics, can cause itching and rash in the genital region.
3. Hormonal Changes
- Menopause: Decreased estrogen levels can lead to vaginal dryness and itching.
- Pregnancy: Hormonal fluctuations during pregnancy may cause increased sensitivity and itching in the genital area.
Symptoms Associated with Genital Pruritus
While itching is the primary symptom, genital pruritus may be accompanied by:
- Redness and Swelling: Inflammation of the affected area.
- Discharge: Unusual vaginal or penile discharge, varying in color and consistency.
- Pain or Burning Sensation: Especially during urination or sexual intercourse.
- Visible Lesions or Sores: Such as blisters, ulcers, or white patches.
Diagnosis of Genital Pruritus
Accurate diagnosis is essential for effective treatment. Healthcare providers may employ the following approaches:
- Medical History and Physical Examination: Assessing symptoms, sexual history, and inspecting the affected area.
- Laboratory Tests: Including swabs, cultures, or blood tests to identify infections or other conditions.
- Skin Biopsy: In cases where dermatological conditions are suspected, a small skin sample may be examined microscopically.
Treatment Options
Treatment strategies depend on the underlying cause:
1. Medications
- Antifungal Agents: For yeast infections, topical or oral antifungal medications are prescribed.
- Antibiotics: Bacterial infections like bacterial vaginosis or certain STIs may require antibiotic therapy.
- Antiviral Medications: Conditions such as genital herpes are managed with antiviral drugs to reduce symptoms and transmission risk.
- Topical Steroids: Dermatological conditions like lichen sclerosus or lichen simplex chronicus may respond to corticosteroid creams.
2. Lifestyle and Home Remedies
- Avoid Irritants: Use gentle, fragrance-free soaps and detergents; avoid douching and wearing tight-fitting clothing.
- Maintain Hygiene: Keep the genital area clean and dry, changing out of wet clothing promptly.
- Use Moisturizers: Apply recommended moisturizers to prevent dryness, especially in cases like vulvar dermatitis.
Prevention Strategies
To reduce the risk of developing genital pruritus:
- Practice Safe Sex: Use condoms and have regular STI screenings.
- Wear Breathable Fabrics: Opt for cotton underwear and avoid synthetic materials that trap moisture.
- Manage Stress: Stress can exacerbate certain skin conditions; incorporating stress-reduction techniques may be beneficial.
When to Seek Medical Attention
Consult a healthcare provider if:
- Symptoms Persist: Itching lasts more than a few days despite home care.
- Severe Discomfort: Pain, swelling, or open sores develop.
- Unusual Discharge: Noticeable changes in color, consistency, or odor of discharge.
- Recurring Symptoms: Frequent episodes of genital itching occur.