Gastrointestinal candidiasis is a fungal infection caused by the overgrowth of Candida species, particularly Candida albicans, within the digestive tract. While Candida organisms are typically harmless commensals in the human gastrointestinal (GI) system, certain conditions can precipitate their proliferation, leading to symptomatic infections.
Etiology and Predisposing Factors
Several factors can disrupt the balance of the gut microbiota, facilitating Candida overgrowth:
- Antibiotic Therapy: Broad-spectrum antibiotics can indiscriminately eliminate beneficial bacteria, reducing microbial competition and allowing Candida to thrive.
- Immunosuppression: Individuals with compromised immune systems, such as those with HIV/AIDS, undergoing chemotherapy, or on immunosuppressive medications, are at heightened risk.
- Metabolic Disorders: Conditions like diabetes mellitus can alter the internal environment, promoting fungal growth.
- Dietary Factors: Diets high in sugar and refined carbohydrates can encourage Candida proliferation.
Clinical Manifestations
The presentation of gastrointestinal candidiasis varies depending on the affected region:
- Esophageal Candidiasis: Symptoms include painful swallowing (odynophagia), difficulty swallowing (dysphagia), and retrosternal pain.
- Gastric Candidiasis: Patients may experience nausea, vomiting, epigastric pain, and bloating.
- Intestinal Candidiasis: Manifestations can include diarrhea, abdominal cramping, and signs of malabsorption such as weight loss and nutrient deficiencies.
Diagnostic Approach
Accurate diagnosis is essential for effective management:
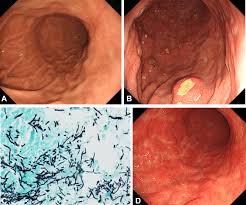
- Endoscopic Evaluation: Direct visualization and biopsy during endoscopy can identify characteristic lesions and facilitate histopathological examination.
- Microbiological Studies: Culturing biopsy samples or stool specimens can confirm Candida overgrowth.
- Laboratory Tests: Assessing for underlying conditions such as diabetes or immunodeficiency is crucial.
Therapeutic Strategies
Management involves a multifaceted approach:
- Antifungal Agents: Medications such as fluconazole or nystatin are commonly prescribed to eradicate the infection.
- Dietary Modifications: Reducing intake of sugars and refined carbohydrates can limit nutrient sources for Candida.
- Probiotics: Supplementation can help restore healthy gut flora, re-establishing microbial balance.
- Addressing Underlying Conditions: Effective management of predisposing factors, such as controlling blood glucose levels in diabetics, is vital.
Prevention and Prognosis
Preventive measures focus on maintaining a balanced microbiome and robust immune function:
- Prudent Antibiotic Use: Limiting unnecessary antibiotic prescriptions can preserve beneficial bacterial populations.
- Immune Support: Adopting a healthy lifestyle, including proper nutrition and stress management, supports immune health.
With timely and appropriate treatment, the prognosis for gastrointestinal candidiasis is generally favorable. However, delayed intervention or persistent underlying risk factors can lead to recurrent or severe infections.
In conclusion, gastrointestinal candidiasis is a condition resulting from an imbalance in the gut’s microbial environment, often precipitated by identifiable risk factors. Recognizing symptoms early and implementing comprehensive treatment strategies are essential for effective management and prevention of recurrence.