Gastritis refers to the inflammation of the stomach lining, a condition that can manifest suddenly (acute gastritis) or develop gradually over time (chronic gastritis). This inflammation disrupts the stomach’s protective barrier, leading to various gastrointestinal symptoms. Understanding the underlying causes, recognizing the symptoms, and seeking appropriate treatment are essential steps in managing this condition effectively.
Causes of Gastritis
Several factors can contribute to the development of gastritis:
- Helicobacter pylori Infection: A prevalent bacterial infection that damages the stomach lining, leading to inflammation.
- Regular Use of Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Medications such as ibuprofen and naproxen can irritate the stomach lining, especially when used frequently or in high doses.
- Excessive Alcohol Consumption: Alcohol can erode the stomach lining, increasing susceptibility to inflammation.
- Stress: Severe physical stress from major surgery, injury, burns, or infections can trigger acute gastritis.
- Autoimmune Disorders: Conditions where the immune system attacks the stomach lining, leading to chronic inflammation.
- Other Diseases and Conditions: Gastritis can be associated with other medical conditions such as HIV/AIDS, Crohn’s disease, celiac disease, sarcoidosis, and parasitic infections.
Symptoms of Gastritis
The presentation of gastritis can vary, with some individuals remaining asymptomatic. Common symptoms include:
- Abdominal Pain: A gnawing or burning ache in the upper abdomen that may improve or worsen with eating.
- Nausea and Vomiting: A sensation of unease in the stomach, sometimes leading to vomiting.
- Bloating: A feeling of fullness or swelling in the upper abdomen.
- Loss of Appetite: Reduced desire to eat, potentially leading to unintentional weight loss.
- Belching and Flatulence: Increased burping and passing gas.
- Indigestion (Dyspepsia): Discomfort or pain in the upper abdomen, often accompanied by a feeling of fullness.
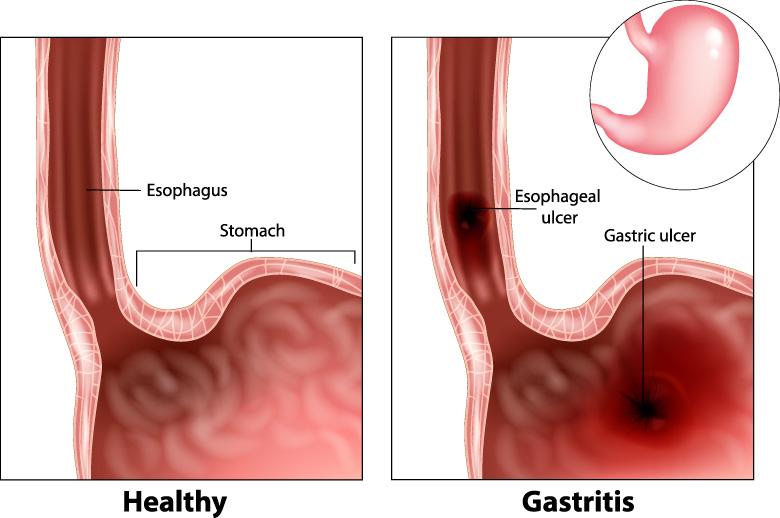
In severe cases, symptoms such as vomiting blood, black or tarry stools, and severe stomach pain may occur, indicating potential complications like bleeding ulcers.
Diagnosis of Gastritis
Accurate diagnosis is crucial for effective management. Healthcare professionals may employ the following diagnostic methods:
- Medical History and Physical Examination: Assessing symptoms, medication use, dietary habits, and lifestyle factors.
- Tests for H. pylori Infection: Stool tests or breath tests to detect the presence of H. pylori bacteria.
- Endoscopy: A procedure involving a thin, flexible tube with a camera to visualize the stomach lining and obtain tissue samples if necessary.
- Imaging Studies: X-rays of the upper digestive system, sometimes using a barium swallow, to identify abnormalities.
Treatment Options for Gastritis
Treatment strategies depend on the underlying cause and severity of the condition:
- Antibiotic Therapy: For H. pylori infections, a combination of antibiotics is prescribed to eradicate the bacteria.
- Medications to Reduce Stomach Acid: Proton pump inhibitors (PPIs) and H2 blockers decrease acid production, allowing the stomach lining to heal.
- Antacids: Over-the-counter antacids can neutralize existing stomach acid, providing symptomatic relief.
- Lifestyle Modifications: Avoiding irritants such as NSAIDs, alcohol, and spicy foods; managing stress; and eating smaller, more frequent meals.
- Treatment of Underlying Conditions: Addressing associated diseases or conditions contributing to gastritis.
In cases where gastritis is caused by prolonged use of NSAIDs or excessive alcohol consumption, discontinuing these substances is essential for healing.