Eubacterium peritonitis is a rare but serious intra-abdominal infection caused by Eubacterium species, a genus of anaerobic, Gram-positive bacteria. This condition primarily affects individuals undergoing peritoneal dialysis (PD) but can also result from gastrointestinal perforations, trauma, or post-surgical complications. Due to its rarity and unique microbiological characteristics, early diagnosis and targeted treatment are essential for preventing severe complications.
Causes and Pathophysiology
Eubacterium species are part of the normal gut microbiota but can become pathogenic when they translocate into the peritoneal cavity due to:
- Gastrointestinal perforation – Ulceration, diverticulitis, or ischemia can lead to bacterial leakage into the peritoneal space.
- Peritoneal Dialysis (PD)-related infections – Contamination during PD exchanges or catheter-related infections.
- Abdominal trauma or post-surgical complications – Bowel perforation or anastomotic leakage after surgery.
- Bacteremia leading to secondary peritonitis – Systemic infections spreading to the peritoneal cavity.
Mechanism of Infection
Eubacterium peritonitis initiates an inflammatory cascade leading to peritoneal irritation, immune activation, and, if untreated, systemic complications such as septic shock.
Clinical Symptoms
The presentation of Eubacterium peritonitis varies but commonly includes:
- Severe abdominal pain – Often diffuse and progressively worsening.
- Fever and chills – Indicative of systemic infection.
- Nausea and vomiting – Due to peritoneal irritation.
- Peritoneal Dialysis complications – Cloudy dialysate, increased white blood cell count.
- Hypotension and tachycardia – Signs of systemic inflammatory response syndrome (SIRS) and possible sepsis.
Diagnosis
Prompt and accurate diagnosis is crucial to manage Eubacterium peritonitis effectively.
Laboratory Tests
- Peritoneal Fluid Analysis
- Elevated WBC count (>100 cells/µL)
- Predominance of neutrophils
- Cloudy appearance
- Microbiological Cultures
- Anaerobic culture of peritoneal fluid
- Identification using molecular techniques (PCR, MALDI-TOF MS)
- Blood Tests
- Elevated C-reactive protein (CRP)
- Increased procalcitonin levels
- Positive blood cultures in systemic infections
- Imaging Studies
- Abdominal CT scan – To identify abscesses, perforations, or inflammation.
- Ultrasound – Useful in peritoneal dialysis-associated peritonitis.
Treatment Strategies
Management of Eubacterium peritonitis includes a combination of antibiotic therapy, supportive care, and potential surgical intervention.
Antibiotic Therapy
- Empirical Treatment (Before culture results):
- Broad-spectrum antibiotics: Piperacillin-tazobactam, Metronidazole, or Carbapenems.
- Definitive Treatment (After bacterial identification):
- Metronidazole or Clindamycin – Highly effective against anaerobic bacteria.
- Beta-lactamase inhibitors – If polymicrobial infection is suspected.
Supportive Care
- Fluid resuscitation – To manage sepsis and prevent hypotension.
- Pain management – Using analgesics.
- Nutritional support – Enteral or parenteral nutrition if bowel dysfunction occurs.
Surgical Intervention
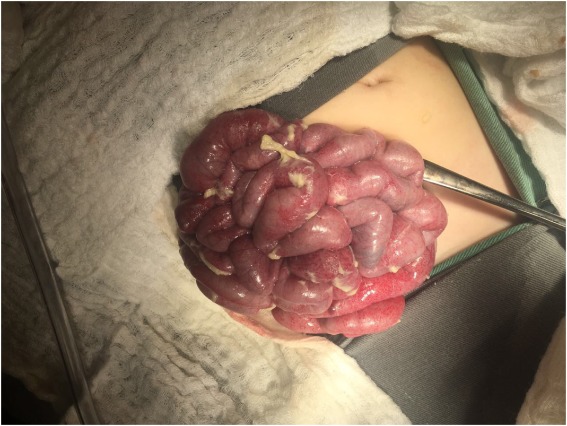
In cases with perforation, abscess formation, or severe infection, surgical management may be necessary:
- Laparotomy or laparoscopic intervention – To drain abscesses and repair perforations.
- Peritoneal Dialysis Catheter Removal – If PD-related peritonitis does not resolve with antibiotics.
Prognosis and Complications
Timely treatment generally leads to a good prognosis. However, delayed intervention can result in:
- Septic shock – Life-threatening if untreated.
- Multisystem organ failure – Due to prolonged infection.
- Peritoneal fibrosis – Chronic inflammation leading to encapsulating peritoneal sclerosis.
Prevention Strategies
- Strict Peritoneal Dialysis Hygiene – Use of sterile techniques to prevent catheter contamination.
- Early Detection of GI Perforations – Prompt surgical intervention in high-risk patients.
- Prophylactic Antibiotics in High-Risk Surgeries – To minimize the risk of intra-abdominal infections.
- Regular Follow-ups for Dialysis Patients – Early detection of catheter-related infections.