Ethylene glycol toxicity is a severe and potentially fatal poisoning resulting from ingestion of ethylene glycol, a common ingredient in antifreeze. Due to its sweet taste, it is particularly hazardous to children and pets. This article explores the toxic effects, clinical manifestations, and treatment strategies for ethylene glycol poisoning.
What is Ethylene Glycol?
Ethylene glycol (C₂H₆O₂) is a colorless, odorless liquid used in antifreeze, industrial solvents, and hydraulic fluids. While useful in various applications, its ingestion leads to severe toxicity due to its metabolism into toxic compounds.
Mechanism of Toxicity
The primary toxic effect of ethylene glycol results from its metabolism in the liver by alcohol dehydrogenase (ADH) into harmful metabolites:
- Glycolic acid contributes to metabolic acidosis.
- Oxalic acid binds calcium, forming insoluble calcium oxalate crystals that damage the kidneys.
Symptoms of Ethylene Glycol Poisoning
The toxicity progresses through three clinical stages:
Stage 1: Neurological Phase (0-12 Hours Post-Ingestion)
- Drunken-like behavior (euphoria, confusion, ataxia)
- Slurred speech
- Nausea and vomiting
- Seizures (in severe cases)
Stage 2: Cardiopulmonary Phase (12-24 Hours Post-Ingestion)
- Tachycardia (rapid heartbeat)
- Hypertension or hypotension
- Hyperventilation (due to metabolic acidosis)
- Pulmonary edema
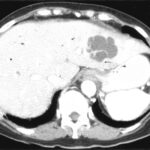
Stage 3: Renal Phase (24-72 Hours Post-Ingestion)
- Acute kidney injury (flank pain, hematuria)
- Oliguria or anuria (low or no urine output)
- Elevated blood urea nitrogen (BUN) and creatinine levels
- Possible multi-organ failure
Diagnosis of Ethylene Glycol Toxicity
Timely diagnosis is critical for effective treatment. Key diagnostic methods include:
1. Clinical History & Examination
- Suspected ingestion of antifreeze
- Presence of neurological, cardiopulmonary, and renal symptoms
2. Laboratory Tests
- Serum Ethylene Glycol Levels: Direct measurement (if available)
- Anion Gap Metabolic Acidosis: High anion gap (>12) with low bicarbonate
- Osmolar Gap: Elevated due to unmetabolized ethylene glycol
- Calcium Oxalate Crystals in Urine: Indicative of kidney involvement
Treatment of Ethylene Glycol Poisoning
1. Immediate Stabilization
- Airway management in unconscious patients
- IV fluids for hydration and electrolyte correction
- Sodium bicarbonate for acidosis correction
2. Antidotal Therapy
- Fomepizole (preferred) or Ethanol: Inhibit alcohol dehydrogenase, preventing toxic metabolite formation
- Pyridoxine (Vitamin B6) & Thiamine (Vitamin B1): Aid alternative metabolism pathways
3. Enhanced Elimination
- Hemodialysis: Effective for severe cases with renal failure, severe acidosis, or high ethylene glycol levels (>50 mg/dL)
4. Supportive Care
- Continuous monitoring of renal function, electrolyte levels, and acid-base status
- Symptom management including anti-seizure medications if needed
Prevention of Ethylene Glycol Toxicity
- Proper Storage: Keep antifreeze and similar chemicals in locked cabinets
- Use of Bittering Agents: Many antifreeze formulations now contain denatonium benzoate to deter ingestion
- Immediate Veterinary Care for Pets: Ethylene glycol is highly toxic to cats and dogs
Prognosis and Long-Term Effects
The prognosis depends on early recognition and treatment. If treated within 8-12 hours, most patients recover without lasting damage. However, delayed treatment can result in permanent renal damage, neurological impairment, or death.