Babesiosis is a parasitic infection caused by protozoa of the genus Babesia. This tick-borne disease predominantly affects red blood cells and poses significant health risks, particularly to individuals with compromised immune systems. Our in-depth exploration of babesiosis aims to provide readers with detailed insights into its causes, symptoms, diagnostic methods, treatments, and preventive strategies.
What Is Babesiosis?
Babesiosis is a zoonotic disease primarily transmitted to humans through the bite of infected ticks, particularly the black-legged tick (Ixodes scapularis). The condition is caused by microscopic parasites, with Babesia microti being the most common species affecting humans in the United States. This parasitic infection disrupts red blood cells, leading to a range of health complications, including hemolytic anemia.
Causes and Transmission
1. Tick-Borne Transmission
- The black-legged tick is the primary vector of babesiosis.
- Ticks typically acquire the parasite by feeding on infected rodents, such as the white-footed mouse.
- Humans contract the disease when bitten by an infected tick during its nymph stage, usually in spring and summer.
2. Other Routes of Transmission
- Blood Transfusion: Transfusion of infected blood products is a notable non-tick transmission method.
- Congenital Transmission: Rare cases of mother-to-child transmission have been reported.
Geographic Distribution
Babesiosis is most prevalent in regions such as the northeastern and upper Midwestern United States, but cases have been reported worldwide.
Symptoms of Babesiosis
The severity of babesiosis symptoms varies, ranging from asymptomatic infections to severe, life-threatening conditions. Common symptoms include:
- Flu-Like Symptoms: Fever, chills, sweats, and muscle aches.
- Fatigue: Persistent tiredness and malaise.
- Hemolytic Anemia: Caused by the destruction of red blood cells, leading to jaundice and dark urine.
- Neurological Symptoms: In rare cases, severe headaches, confusion, or even seizures.
High-Risk Groups
- Individuals over 50 years old.
- People with compromised immune systems (e.g., due to HIV, cancer, or organ transplantation).
- Patients lacking a spleen (asplenia).
Diagnosing
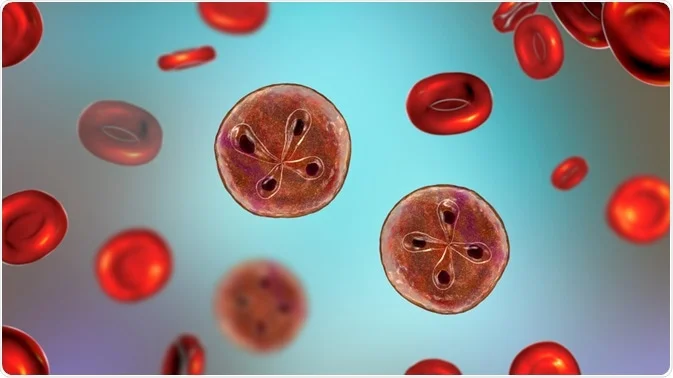
1. Blood Smear Analysis
Microscopic examination of blood smears can reveal Babesia parasites within red blood cells.
2. Polymerase Chain Reaction (PCR)
PCR testing is a sensitive method to detect Babesia DNA in the blood.
3. Serology Tests
Antibody detection tests, such as indirect immunofluorescence assay (IFA), help confirm babesiosis.
4. Complete Blood Count (CBC)
Abnormal CBC results, such as anemia or thrombocytopenia, may indicate babesiosis.
Treatment Options for Babesiosis
1. Combination Therapy
- Atovaquone and Azithromycin: The first-line treatment for mild to moderate babesiosis.
- Clindamycin and Quinine: Often reserved for severe cases.
2. Supportive Care
Patients with severe babesiosis may require:
- Blood transfusions.
- Intravenous fluids.
- Hospitalization for intensive monitoring.
Preventing
1. Avoiding Tick Bites
- Protective Clothing: Wear long sleeves and pants in wooded or grassy areas.
- Tick Repellents: Use products containing DEET or permethrin.
- Regular Tick Checks: Inspect skin and clothing after outdoor activities.
2. Environmental Management
- Maintain well-trimmed lawns and remove leaf litter to reduce tick habitats.
- Treat outdoor areas with acaricides to minimize tick populations.
3. Blood Screening
- Ensure blood donors are screened for Babesia to prevent transfusion-associated transmission.
Public Health
Babesiosis is a growing public health concern due to its increasing incidence in endemic areas and its potential for severe outcomes. Enhanced public awareness, robust diagnostic protocols, and effective preventive measures are critical to managing the disease’s impact.
Lifecycle
Stay informed about babesiosis and take proactive measures to safeguard your health. Early detection and timely treatment are vital in managing this potentially serious condition.
myhealthmag

