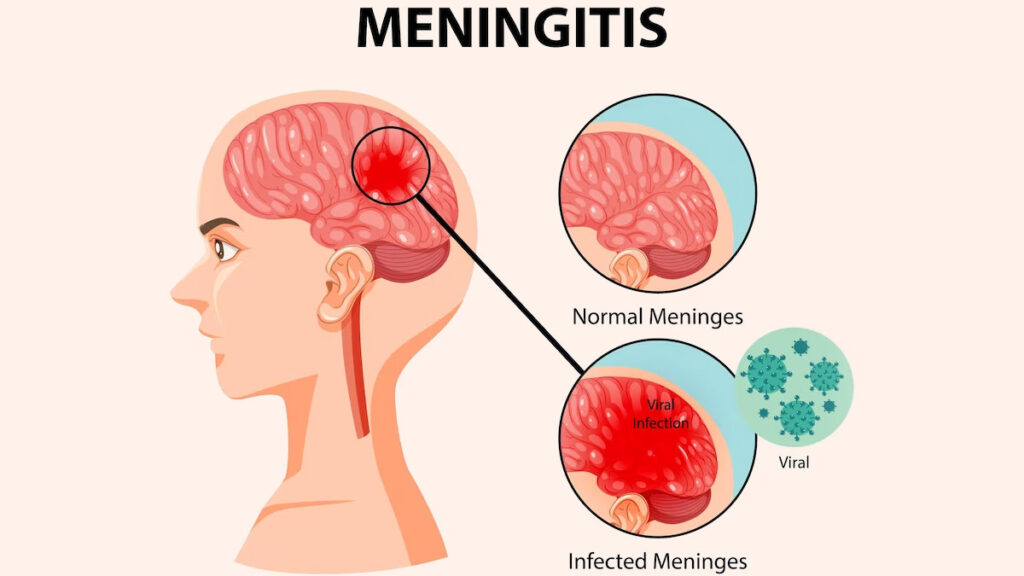
Escherichia coli (E. coli) meningitis is a life-threatening bacterial infection that primarily affects neonates and immunocompromised individuals. It is a leading cause of neonatal meningitis, particularly in preterm infants. The E. coli K1 strain is responsible for the majority of cases due to its enhanced ability to penetrate the blood-brain barrier (BBB).
Causes and Risk Factors
1. Bacterial Transmission
- Vertical Transmission: From mother to infant during birth (ascending infection, chorioamnionitis, or premature rupture of membranes).
- Nosocomial Transmission: Infection acquired in neonatal intensive care units (NICUs).
- Hematogenous Spread: Bacteria enter the bloodstream and cross the BBB.
2. Risk Factors
- Prematurity and low birth weight
- Maternal infections (urinary tract infections, chorioamnionitis)
- Immunosuppression or congenital defects
- Use of invasive medical devices (e.g., catheters, mechanical ventilation)
Pathogenesis of E. Coli Meningitis
The pathophysiology involves several steps:
- Colonization: E. coli K1 adheres to intestinal or vaginal mucosa.
- Bacteremia: Bacteria invade the bloodstream and evade immune responses.
- BBB Invasion: E. coli K1 crosses the BBB using molecular mimicry.
- CSF Infection: The bacteria proliferate in the cerebrospinal fluid (CSF).
- Inflammatory Response: Immune activation leads to increased intracranial pressure and neuronal damage.
Clinical Presentation
Neonates:
- Poor feeding, lethargy, irritability
- Respiratory distress, apnea
- Hypothermia or fever
- Bulging fontanelle (late-stage)
- Seizures
Adults (Rare Cases):
- High fever, neck stiffness
- Severe headache, photophobia
- Altered mental status, confusion
- Seizures
Diagnosis of E. Coli Meningitis
1. Lumbar Puncture and CSF Analysis
- Elevated White Blood Cell (WBC) Count (>1000/mm³)
- Low Glucose Levels (<40 mg/dL)
- Elevated Protein Levels (>100 mg/dL)
- Gram Staining & Culture: Gram-negative rods
2. Blood Culture
- Identifies E. coli in the bloodstream
- Confirms antibiotic susceptibility
3. Imaging (CT/MRI)
- Detects complications (ventriculitis, hydrocephalus)
Treatment and Management
1. Empirical Antibiotic Therapy
- First-Line:
- Cefotaxime + Ampicillin (neonates)
- Ceftriaxone (older children/adults)
- Resistant Strains:
- Meropenem (if ESBL-producing E. coli)
- Colistin (for multidrug-resistant strains)
2. Supportive Care
- Intravenous Fluids to maintain hydration
- Mechanical Ventilation if respiratory distress occurs
- Seizure Control (e.g., Phenobarbital)
Complications and Prognosis
Short-Term Complications
- Septic shock
- Brain abscess formation
- Hydrocephalus
Long-Term Neurological Sequelae
- Cognitive impairments
- Sensorineural hearing loss
- Developmental delays
Prevention Strategies
- Maternal Screening: Detect and treat maternal infections during pregnancy
- Intrapartum Antibiotics: Prophylaxis for high-risk pregnancies
- Neonatal Sepsis Protocols: Early identification and intervention in NICUs