Erythroid leukemia, also known as acute erythroid leukemia (AEL) or erythroleukemia, is a rare and aggressive subtype of acute myeloid leukemia (AML). It primarily affects the erythroid precursor cells responsible for red blood cell production in the bone marrow. This malignancy leads to ineffective hematopoiesis, severe anemia, and systemic complications.
Pathophysiology of Erythroid Leukemia
Erythroid leukemia arises from the uncontrolled proliferation of abnormal erythroblasts in the bone marrow. This results in the suppression of normal blood cell production, leading to cytopenias and bone marrow failure.
Causes and Risk Factors
While the exact etiology of erythroid leukemia remains unclear, several factors contribute to its development:
- Genetic Mutations: TP53, NPM1, and FLT3 mutations
- Myelodysplastic Syndromes (MDS): Can evolve into AEL
- Chemical Exposure: Benzene and chemotherapy agents
- Radiation Exposure: High-dose ionizing radiation
- Viral Infections: Potential association with human T-cell leukemia virus (HTLV-1)
Clinical Manifestations
Patients with erythroid leukemia present with nonspecific but severe symptoms, including:
- Profound Anemia: Fatigue, pallor, shortness of breath
- Thrombocytopenia: Easy bruising, petechiae, prolonged bleeding
- Leukopenia: Increased susceptibility to infections
- Hepatosplenomegaly: Enlarged liver and spleen due to extramedullary hematopoiesis
- Bone Pain: Resulting from marrow expansion
Diagnostic Criteria
Blood Tests and Bone Marrow Examination
- Complete Blood Count (CBC): Severe anemia, thrombocytopenia, leukopenia
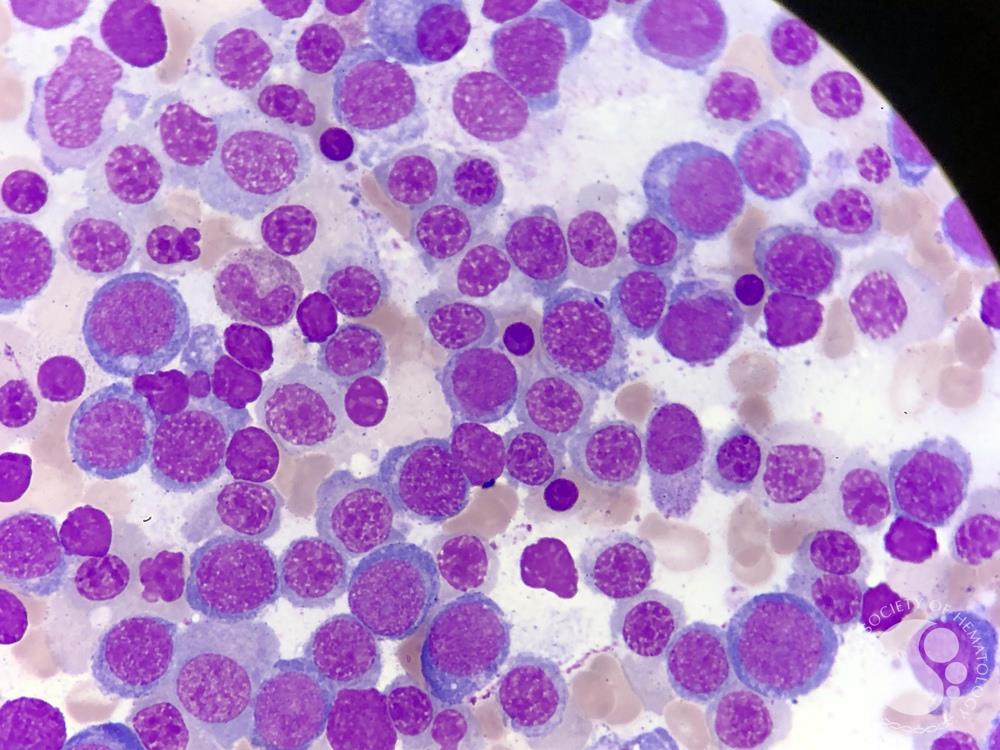
- Peripheral Blood Smear: Abnormal erythroblasts, dysplastic changes
- Bone Marrow Biopsy:
- Hypercellular marrow with >50% erythroid precursors
- Blasts comprising >20% of non-erythroid cells (WHO 2016 criteria)
Cytogenetic and Molecular Testing
- Flow Cytometry: Confirms aberrant erythroid markers (CD71, glycophorin A)
- Genetic Studies: TP53, ASXL1, and RUNX1 mutations detected via PCR or next-gen sequencing
- Cytogenetic Analysis: Complex karyotypes with frequent chromosomal abnormalities
Differential Diagnosis
Erythroid leukemia must be distinguished from other bone marrow disorders, such as:
- Myelodysplastic syndromes (MDS) with excess blasts
- Pure erythroid leukemia (PEL) (a rare, aggressive subtype)
- Other AML subtypes with erythroid differentiation
Treatment Strategies
Induction Therapy
- 7+3 Chemotherapy: Standard AML regimen (Cytarabine + Daunorubicin)
- Hypomethylating Agents: Azacitidine or Decitabine for elderly patients
Consolidation Therapy
- Allogeneic Stem Cell Transplant (SCT): Preferred for high-risk patients
- Targeted Therapies: FLT3 inhibitors (Midostaurin), IDH inhibitors (Enasidenib)
Supportive Care
- Blood Transfusions: For severe anemia
- Antimicrobial Prophylaxis: To prevent infections
- Growth Factors: Erythropoietin-stimulating agents (ESAs) in select cases
Prognosis and Survival Rates
Erythroid leukemia has a poor prognosis, with median overall survival (OS) of 6–12 months in untreated cases. Prognostic factors include:
- Cytogenetic Profile: Complex karyotypes indicate worse outcomes
- Age & Comorbidities: Older patients have lower survival rates
- Response to Therapy: Poor responders to induction therapy have higher relapse rates