Overview of B. fragilis Infection
Bacteroides fragilis, a Gram-negative anaerobic bacterium, is an essential component of the human gut microbiota. While it generally maintains a symbiotic relationship with its host, it can cause opportunistic infections under certain conditions, particularly when the mucosal barrier is compromised. These infections are often serious and require prompt medical attention.

Understanding Bacteroides fragilis
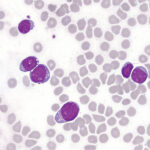
Characteristics of Bacteroides fragilis
- Gram-negative rod: Stains pink under Gram staining due to its thin peptidoglycan layer.
- Anaerobic metabolism: Thrives in environments devoid of oxygen.
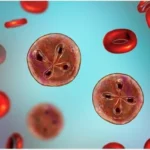
- Capsule formation: Enables immune evasion and contributes to abscess formation.
- Beta-lactamase production: Confers resistance to beta-lactam antibiotics, making treatment challenging.
Role in the Gut Microbiota
B. fragilis plays a crucial role in maintaining gut homeostasis, aiding in digestion, and modulating the immune system. However, its pathogenic potential is activated when it translocates to sterile areas of the body, leading to infection.
Causes and Risk Factors
Primary Causes
- Mucosal barrier disruption: Trauma, surgery, or diseases like inflammatory bowel disease can allow B. fragilis to invade sterile body sites.
- Immunosuppression: Conditions such as HIV, cancer, or the use of immunosuppressive drugs increase susceptibility.
Common Risk Factors
- Abdominal surgery or trauma
- Appendicitis
- Diverticulitis
- Pelvic inflammatory disease
- Use of invasive devices like catheters
Symptoms of B. fragilis Infection
The clinical presentation varies based on the site of infection. Common symptoms include:
- Abdominal pain: Often linked to intra-abdominal abscesses.
- Fever: A systemic response to infection.
- Localized swelling or tenderness: Suggestive of abscess formation.
- Sepsis: In severe cases, systemic inflammatory response may occur.
Diagnosis
Laboratory Investigations
- Specimen Collection: Aspirates or biopsies from abscesses, blood cultures for systemic infections.
- Microscopy and Staining: Identification of Gram-negative rods.
- Anaerobic Culture: Isolation of B. fragilis in specific media under anaerobic conditions.
Imaging Techniques
- CT Scan: Useful for identifying abscesses.
- Ultrasound: A non-invasive option for localized infections.
Treatment
Antibiotic Therapy
- First-line agents: Metronidazole or beta-lactam/beta-lactamase inhibitor combinations.
- Alternative options: Carbapenems or clindamycin.
- Resistance management: Monitor for beta-lactamase production and adjust therapy accordingly.
Surgical Intervention
- Drainage of abscesses or debridement of infected tissues may be necessary to achieve complete resolution.
Complications
- Abscess formation: A hallmark of anaerobic infections.
- Peritonitis: Severe abdominal infection due to perforation or leakage.
- Sepsis and septic shock: Potentially life-threatening systemic responses.
Prevention
- Aseptic surgical techniques: To minimize the risk of infection.
- Prompt treatment of primary infections: Prevents secondary complications.
- Judicious use of antibiotics: Reduces resistance development.
Prognosis
With early and appropriate treatment, the prognosis is generally favorable. Delayed treatment or mismanagement can lead to severe complications and increased mortality rates.
Pathogenesis of B. fragilis Infection
B. fragilis infections, though uncommon, require timely diagnosis and treatment to prevent severe outcomes. Understanding the bacterium’s dual role as both a commensal and pathogen highlights the importance of maintaining gut health and promptly addressing risk factors.