Lupus nephritis is a severe manifestation of systemic lupus erythematosus (SLE), characterized by inflammation of the kidneys. Active lupus nephritis demands timely diagnosis and management to prevent progressive renal damage and long-term complications. This article explores the causes, symptoms, diagnostic approaches, and treatment modalities for active lupus nephritis.
Understanding Active Lupus Nephritis
Active lupus nephritis occurs when the immune system attacks the kidneys, leading to inflammation and impaired renal function. The condition is most common in patients with systemic lupus erythematosus and can range in severity from mild kidney inflammation to severe renal failure.
Pathophysiology of Lupus Nephritis
The immune dysregulation in lupus leads to the production of autoantibodies and immune complexes that deposit in the glomeruli. This triggers an inflammatory response, damaging renal tissues and impairing kidney function.
Classification of Lupus Nephritis
The World Health Organization (WHO) and the International Society of Nephrology/Renal Pathology Society (ISN/RPS) classify lupus nephritis into six classes based on histopathology:
- Class I: Minimal mesangial lupus nephritis
- Class II: Mesangial proliferative lupus nephritis
- Class III: Focal lupus nephritis
- Class IV: Diffuse lupus nephritis (most severe form)
- Class V: Membranous lupus nephritis
- Class VI: Advanced sclerosing lupus nephritis
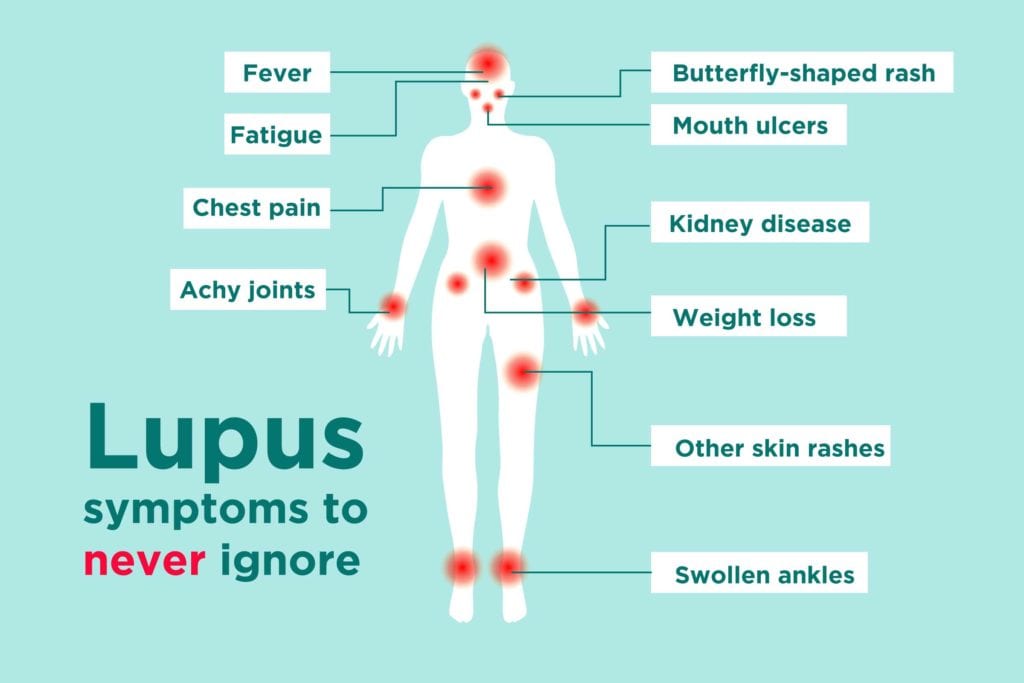
Symptoms
The clinical presentation of lupus nephritis varies, with symptoms ranging from asymptomatic proteinuria to severe renal impairment. Common symptoms include:
- Foamy urine (indicative of proteinuria)
- Hematuria (blood in urine)
- Swelling in the legs, ankles, and feet (edema)
- Elevated blood pressure (hypertension)
- Fatigue and general malaise
Diagnostic Approaches
Early and accurate diagnosis of active lupus nephritis is essential for effective treatment. Key diagnostic methods include:
1. Urine Tests
- Urinalysis: Identifies proteinuria and hematuria.
- 24-hour urine collection: Measures protein levels for more accurate assessment.
2. Blood Tests
- Serum creatinine and blood urea nitrogen (BUN): Indicators of kidney function.
- Complement levels (C3 and C4): Low levels suggest active disease.
- Anti-dsDNA antibodies: Elevated levels correlate with active lupus nephritis.
3. Renal Biopsy
Renal biopsy remains the gold standard for diagnosing lupus nephritis. It helps determine the histological class, which guides treatment decisions.
Treatment Strategies
The management of active lupus nephritis focuses on reducing inflammation, suppressing autoimmunity, and preserving renal function. Treatment is tailored to the disease severity and histological class.
1. Induction Therapy
Induction therapy aims to control active inflammation rapidly. Common options include:
- Corticosteroids: High-dose steroids reduce inflammation.
- Immunosuppressive drugs: Cyclophosphamide and mycophenolate mofetil (MMF) are standard choices.
2. Maintenance Therapy
After induction therapy, maintenance therapy prevents relapses. MMF and azathioprine are commonly used during this phase.
3. Biologic Therapies
Biologic agents, such as belimumab and rituximab, are emerging options for refractory cases or patients intolerant to standard treatments.
4. Supportive Care
Supportive measures are critical to managing complications and maintaining kidney function. These include:
- Blood pressure control with angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs).
- Dietary modifications to limit salt and protein intake.
- Managing co-morbid conditions like diabetes or infections.
Prognosis and Long-term Outcomes
The prognosis for active lupus nephritis depends on early diagnosis, effective treatment, and adherence to therapy. Patients who respond well to induction and maintenance therapy have a good chance of achieving long-term remission. However, severe cases may progress to end-stage renal disease, necessitating dialysis or kidney transplantation.
Active lupus nephritis is a complex and potentially life-threatening condition requiring prompt diagnosis and comprehensive management. By employing tailored therapies and ensuring regular monitoring, healthcare providers can significantly improve patient outcomes and quality of life.