Enterobacter peritonitis is a serious intra-abdominal infection caused by Enterobacter species, commonly Enterobacter cloacae and Enterobacter aerogenes. It often occurs as a complication of peritoneal dialysis (PD), abdominal surgery, or spontaneous bacterial peritonitis (SBP) in patients with liver cirrhosis. Early diagnosis and appropriate antimicrobial therapy are crucial to prevent complications and mortality.
Causes and Risk Factors
Microbial Etiology
Enterobacter species are facultative anaerobic gram-negative bacilli that exhibit multidrug resistance due to their ability to produce beta-lactamases, including extended-spectrum beta-lactamases (ESBLs) and carbapenemases.
Predisposing Factors
- Peritoneal Dialysis (PD): Continuous ambulatory peritoneal dialysis (CAPD) patients have an increased risk due to catheter contamination.
- Abdominal Surgery: Postoperative infections are a significant source of Enterobacter peritonitis.
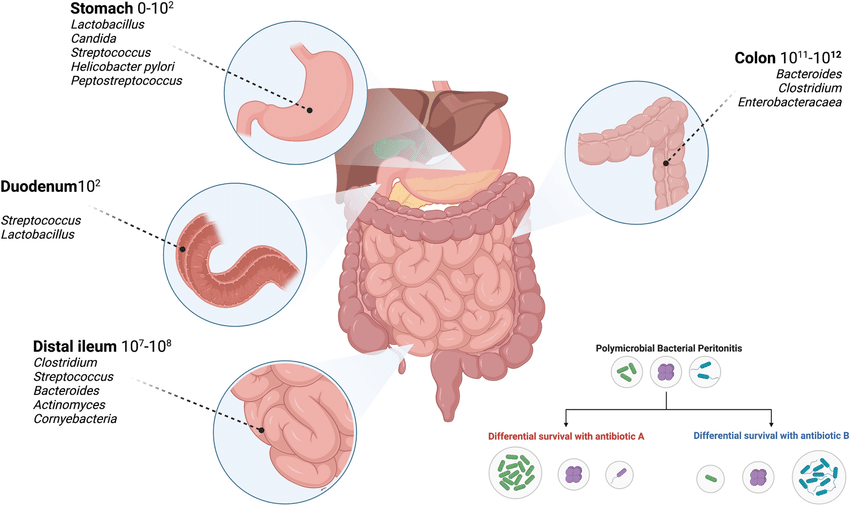
- Gastrointestinal Perforation: Leakage of intestinal contents introduces Enterobacter into the peritoneal cavity.
- Immunosuppression: Patients with diabetes, malignancies, or undergoing chemotherapy are at higher risk.
Clinical Presentation
Patients with Enterobacter peritonitis typically present with:
- Severe Abdominal Pain: Diffuse and persistent pain.
- Fever and Chills: Sign of systemic infection.
- Nausea and Vomiting: Common due to gastrointestinal irritation.
- Cloudy Peritoneal Dialysis Effluent: In CAPD patients, an early diagnostic indicator.
- Rebound Tenderness and Guarding: Indicating peritoneal inflammation.
Diagnosis
Laboratory and Microbiological Testing
- Peritoneal Fluid Analysis:
- White Blood Cell (WBC) Count: >100 cells/µL with >50% polymorphonuclear neutrophils.
- Gram Stain: Identifies gram-negative bacilli.
- Culture and Sensitivity Testing: Confirms Enterobacter species and determines antibiotic susceptibility.
- Blood Cultures: Essential in systemic infections or sepsis suspicion.
- Imaging:
- Ultrasound or CT Scan: Detects intra-abdominal abscesses or perforations.
Treatment and Management
Empirical Antibiotic Therapy
Given Enterobacter‘s resistance mechanisms, therapy should be guided by susceptibility testing. However, empirical treatment often includes:
- Carbapenems (Imipenem, Meropenem): Preferred for ESBL-producing strains.
- Cefepime or Piperacillin-Tazobactam: Alternative options for non-ESBL strains.
- Aminoglycosides (Gentamicin, Amikacin): Used in combination therapy.
- Fluoroquinolones (Ciprofloxacin, Levofloxacin): Considered in non-severe cases.
Supportive Care
- Intravenous Fluids: Maintain hydration and electrolyte balance.
- Pain Management: Use of analgesics as needed.
- Surgical Intervention: Required in cases of abscess formation or bowel perforation.
Prognosis and Complications
Complications
- Sepsis and Septic Shock: A life-threatening condition requiring ICU management.
- Intra-abdominal Abscesses: May require drainage.
- Multidrug Resistance: Leads to treatment failure and prolonged hospitalization.
Prognosis
With early diagnosis and appropriate antibiotic therapy, the prognosis is generally favorable. However, delayed treatment can lead to severe complications and increased mortality.
Prevention Strategies
- Aseptic Technique in Peritoneal Dialysis: Regular hand hygiene and catheter care.
- Prophylactic Antibiotics: Prior to abdominal surgeries.
- Early Detection and Management of Gastrointestinal Conditions: Prevents bacterial translocation.