Enterobacter joint infection is a rare but serious condition caused by Enterobacter species, a group of Gram-negative, facultatively anaerobic bacteria. These infections typically occur in prosthetic joints, post-surgical cases, or immunocompromised individuals. Early detection and prompt intervention are crucial to prevent joint destruction and systemic complications.
Causes and Risk Factors
1. Primary Causes:
- Direct inoculation during joint surgery or trauma
- Hematogenous spread from other infected sites (e.g., urinary tract, respiratory tract)
- Contaminated medical devices or implants
2. Risk Factors:
- Prosthetic joint implantation
- Immunosuppression (diabetes, cancer, chronic kidney disease)
- Recent hospitalization or ICU stay
- Broad-spectrum antibiotic use, leading to resistance
- History of prior joint infections
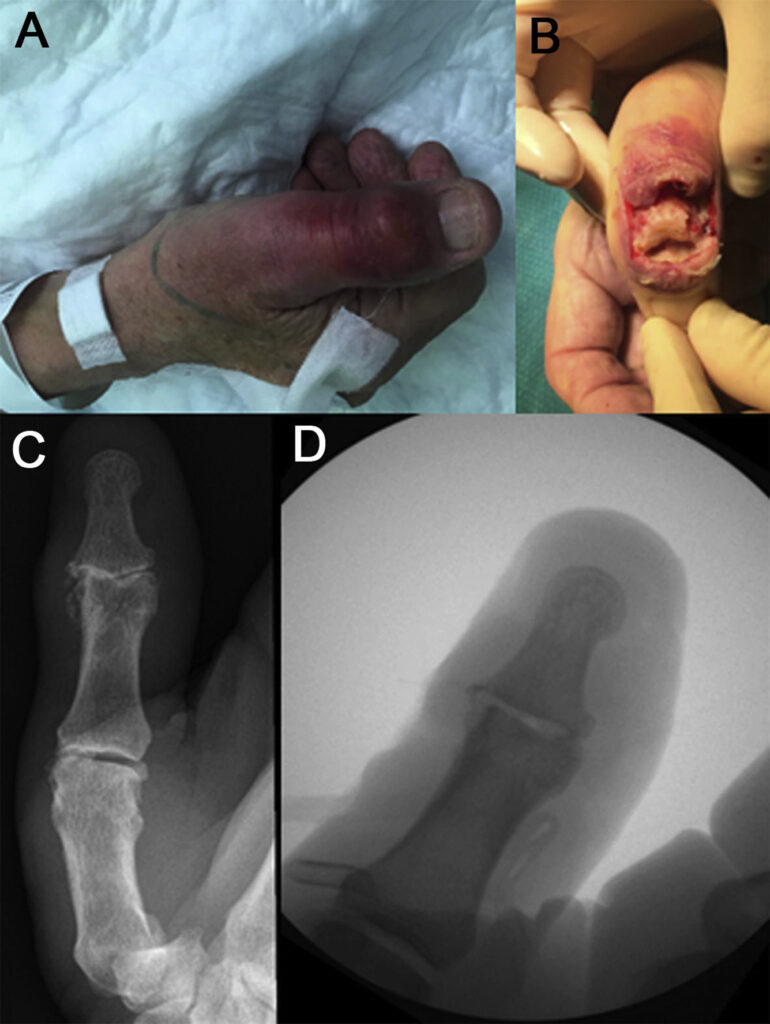
Clinical Presentation
Patients with Enterobacter joint infection often present with:
- Acute or chronic joint pain
- Swelling and erythema around the affected joint
- Limited range of motion
- Fever and systemic signs of infection
- Purulent joint effusion (in septic arthritis cases)
The symptoms may resemble other bacterial joint infections, making laboratory confirmation essential.
Diagnostic Approach
1. Synovial Fluid Analysis
- Gram stain & culture: Detects Enterobacter species
- Leukocyte count >50,000 cells/mm³ suggests septic arthritis
- PCR and 16S rRNA sequencing: Used in culture-negative cases
2. Blood and Tissue Cultures
- Positive blood cultures indicate hematogenous spread
- Joint aspirate and intraoperative tissue sampling improve diagnostic yield
3. Imaging Studies
- X-ray & MRI: Evaluate joint destruction or implant loosening
- Ultrasound: Detects effusions for guided aspiration
Treatment Strategies
1. Antibiotic Therapy
Empirical therapy should be initiated based on resistance patterns and adjusted after culture results.
- First-line: Carbapenems (Meropenem, Imipenem) or Fourth-gen Cephalosporins (Cefepime)
- Alternative: Fluoroquinolones (Ciprofloxacin, Levofloxacin) if susceptible
- Duration: 4-6 weeks for native joints, 6-12 weeks for prosthetic joint infections (PJI)
2. Surgical Management
- Joint Debridement & Lavage: Preferred for early infections
- Prosthesis Removal & Two-Stage Exchange: Standard for chronic PJI
- Arthrodesis or Amputation: Considered in refractory cases
3. Adjunctive Therapies
- Infection Control Measures: Address comorbidities (diabetes, immune suppression)
- Rehabilitation & Physical Therapy: Prevent joint stiffness post-treatment
Prognosis and Prevention
Prognosis
- Early-stage infections treated with timely intervention have a good prognosis.
- Chronic infections often require extensive surgery and prolonged antibiotic therapy.
- Multi-drug resistant (MDR) Enterobacter infections have poorer outcomes.
Preventive Measures
- Strict aseptic techniques during joint surgeries
- Preoperative screening for high-risk patients
- Judicious antibiotic use to prevent resistance
- Regular follow-up for patients with prosthetic joints