Endometritis refers to the inflammation of the endometrium, the inner lining of the uterus, predominantly resulting from infections. Among the various pathogens, Enterobacter species, part of the Enterobacteriaceae family, have been identified as causative agents. This article delves into the etiology, risk factors, clinical manifestations, diagnostic approaches, and treatment modalities associated with Enterobacter-induced endometritis.
Etiology and Pathogenesis
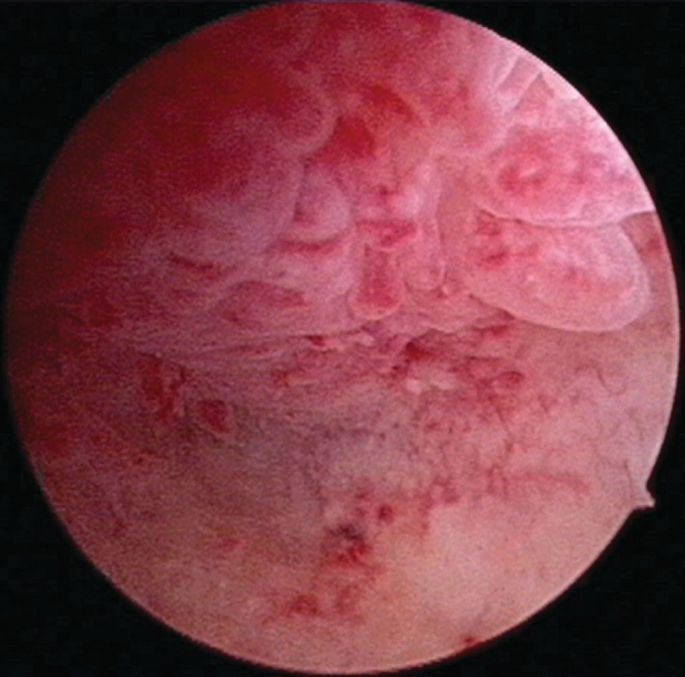
Enterobacter species are Gram-negative bacilli commonly found in the gastrointestinal tract but can act as opportunistic pathogens in the genital tract. In the context of endometritis, these bacteria may ascend from the lower genital tract or be introduced during obstetric or gynecological procedures. The pathogenesis involves bacterial colonization of the endometrium, leading to an inflammatory response characterized by infiltration of neutrophils and plasma cells.
Risk Factors
Several factors predispose individuals to Enterobacter endometritis:
- Obstetric Procedures: Cesarean sections, especially without prophylactic antibiotics, significantly increase the risk.
- Gynecological Interventions: Procedures such as dilation and curettage (D&C), endometrial biopsy, hysteroscopy, or intrauterine device (IUD) placement can introduce bacteria into the uterine cavity.
- Prolonged Labor: Extended labor durations, particularly with multiple vaginal examinations, elevate the risk of infection.
- Premature Rupture of Membranes: Early rupture increases the likelihood of ascending infections.
- Retained Products of Conception: Incomplete expulsion of placental or fetal tissues can serve as a nidus for bacterial growth.
Clinical Manifestations
The presentation of Enterobacter endometritis can vary but commonly includes:
- Fever: Elevated body temperature often exceeding 38°C.
- Pelvic or Lower Abdominal Pain: Persistent discomfort or tenderness.
- Abnormal Vaginal Discharge: Often malodorous and purulent.
- Abnormal Uterine Bleeding: Irregular bleeding patterns, including postcoital or intermenstrual bleeding.
- General Malaise: Symptoms such as fatigue, chills, or a general feeling of unwellness.
Diagnostic Approaches
Accurate diagnosis is crucial for effective management:
- Clinical Evaluation: A thorough history and physical examination, focusing on recent obstetric or gynecological procedures and symptomatology.
- Microbiological Cultures: Obtaining endometrial or cervical samples for culture to identify Enterobacter species.
- Laboratory Tests: Complete blood count (CBC) may reveal leukocytosis; elevated inflammatory markers like C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR) may be present.
- Imaging Studies: While not always necessary, pelvic ultrasound can help identify retained products of conception or abscess formation.
Treatment Modalities
Management of Enterobacter endometritis involves antimicrobial therapy and supportive care:
- Antibiotic Therapy: Empirical broad-spectrum antibiotics should be initiated promptly, later tailored based on culture sensitivities. Regimens may include a combination of clindamycin and gentamicin.
- Surgical Intervention: In cases of abscess formation or retained products, surgical evacuation or drainage may be necessary.
- Supportive Care: Includes analgesics for pain management and monitoring for potential complications.
Prevention Strategies
Preventative measures are essential to reduce the incidence of Enterobacter endometritis:
- Prophylactic Antibiotics: Administering antibiotics prior to cesarean sections or invasive gynecological procedures has been shown to significantly reduce infection rates.
- Aseptic Techniques: Strict adherence to sterile procedures during obstetric and gynecological interventions.
- Timely Removal of Retained Products: Ensuring complete evacuation of the uterine cavity post-delivery or miscarriage.