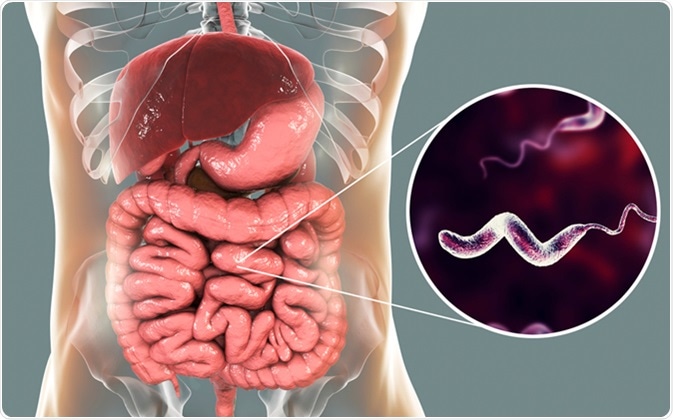
Enteric campylobacteriosis is a significant bacterial infection affecting the gastrointestinal tract, primarily caused by Campylobacter species. Recognized as one of the leading causes of bacterial gastroenteritis worldwide, this infection poses substantial public health challenges due to its prevalence and potential complications.
Etiology and Epidemiology
Causative Agents
The genus Campylobacter comprises several species, with Campylobacter jejuni and Campylobacter coli being the most frequently implicated in human infections. These gram-negative, spiral-shaped bacteria thrive in microaerophilic environments and are commonly found in the intestines of various warm-blooded animals, including poultry, cattle, and swine.
Prevalence
Campylobacter infections are widespread globally. In the United States, the Centers for Disease Control and Prevention (CDC) estimates approximately 1.5 million cases annually. Similarly, the World Health Organization (WHO) identifies Campylobacter as one of the four key global causes of diarrheal diseases, underscoring its substantial impact on public health.
Transmission and Risk Factors
Modes of Transmission
Humans typically acquire Campylobacter infections through:
- Consumption of Contaminated Food or Water: Ingesting undercooked or raw poultry, unpasteurized milk, or contaminated water are common sources.
- Direct Contact: Handling animals carrying the bacteria, especially poultry, without proper hygiene practices.
- Cross-Contamination: Using the same cutting boards or utensils for raw meats and ready-to-eat foods without adequate cleaning.
Risk Factors
Factors increasing the likelihood of infection include:
- Travel to Developing Countries: Exposure to areas with limited sanitation increases risk.
- Occupational Hazards: Individuals working in poultry farming or meat processing industries.
- Age and Immune Status: Young children, the elderly, and immunocompromised individuals are more susceptible to severe infections.
Clinical Manifestations
Symptoms
After an incubation period of approximately 2 to 5 days, infected individuals may experience:
- Diarrhea: Often watery and may contain blood.
- Abdominal Pain and Cramping: Severe and sometimes mimicking appendicitis.
- Fever: Commonly accompanies gastrointestinal symptoms.
- Nausea and Vomiting: Less frequent but possible.
Duration
Symptoms typically persist for about one week. While many cases resolve without medical intervention, some individuals may experience prolonged or severe illness requiring medical attention.
Diagnosis
Accurate diagnosis involves:
- Stool Culture: Isolation of Campylobacter from fecal samples remains the gold standard.
- Molecular Methods: Polymerase Chain Reaction (PCR) assays offer rapid and sensitive detection.
- Antigen Detection Tests: Enzyme immunoassays can identify specific Campylobacter antigens in stool samples.
Treatment
General Management
- Hydration: Oral rehydration solutions are essential to prevent dehydration due to diarrhea.
- Electrolyte Replacement: Maintaining electrolyte balance is crucial, especially in severe cases.
Antibiotic Therapy
Antibiotics are reserved for severe or high-risk cases and may include:
- Macrolides: Erythromycin or azithromycin are often first-line treatments.
- Fluoroquinolones: Such as ciprofloxacin; however, increasing resistance is a concern.
Complications
While most individuals recover fully, potential complications include:
- Guillain-Barré Syndrome (GBS): A rare autoimmune disorder leading to muscle weakness and paralysis. Campylobacter infection is a leading antecedent to GBS.
- Reactive Arthritis: Joint inflammation occurring weeks after the initial infection.
- Bacteremia: Particularly in immunocompromised individuals, the bacteria can enter the bloodstream, leading to systemic infection.
Prevention
Preventative measures encompass:
- Proper Food Handling:
- Thoroughly cook poultry and meat to safe internal temperatures.
- Avoid cross-contamination by using separate utensils and cutting boards for raw and cooked foods.
- Consumption of Pasteurized Products: Always choose pasteurized milk and dairy products.
- Hand Hygiene: Wash hands with soap and water after handling raw meat, contact with animals, and before eating.
- Safe Water Practices: Drink treated or boiled water, especially in areas where water quality is uncertain.