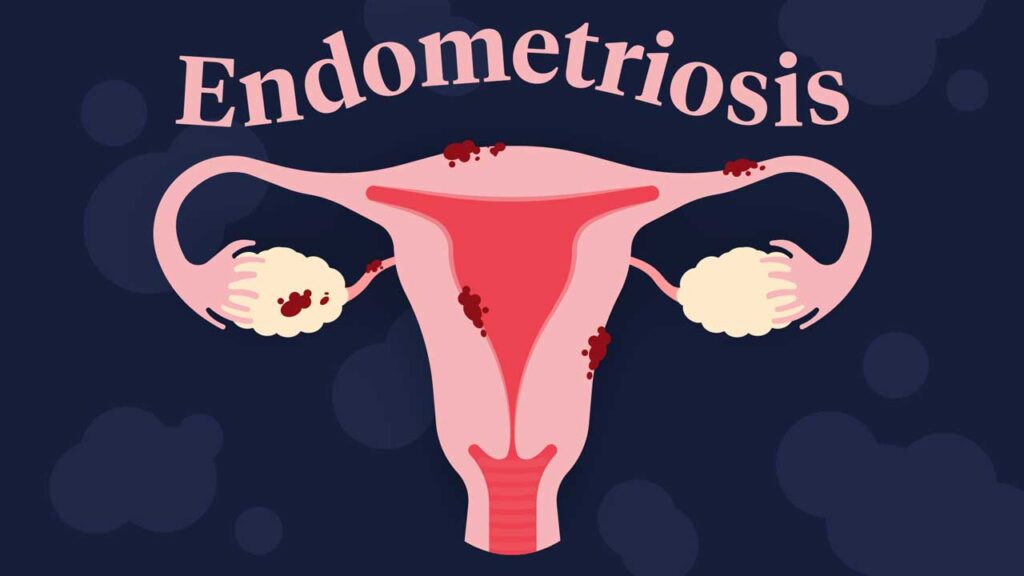
Endometriosis is a chronic gynecological condition where tissue similar to the endometrium—the lining of the uterus—grows outside the uterine cavity. This aberrant growth often leads to significant pain and fertility challenges, affecting approximately 10% of women of reproductive age worldwide. Despite its prevalence, endometriosis remains underdiagnosed, with many individuals enduring symptoms for years before receiving appropriate care.
Symptoms of Endometriosis
The clinical presentation of endometriosis varies, but common symptoms include:
- Pelvic Pain: Chronic pelvic discomfort, often correlating with menstrual cycles, is a hallmark of endometriosis. This pain can be debilitating and impact daily activities.
- Dysmenorrhea: Severe menstrual cramps that may intensify over time, frequently unresponsive to standard pain relief measures.
- Dyspareunia: Pain during or after sexual intercourse, which can strain intimate relationships and affect quality of life.
- Bowel and Urinary Symptoms: Painful bowel movements, urination during menstrual periods, diarrhea, constipation, and bloating are reported by some individuals.
- Infertility: Endometriosis is found in 20% to 40% of women who are infertile, making it a significant factor in reproductive health challenges.
It’s important to note that symptom severity does not always correlate with the extent of the disease; some individuals with advanced endometriosis may experience minimal discomfort, while others with milder forms suffer severe symptoms.
Causes and Risk Factors
The exact etiology of endometriosis remains unclear, but several theories and risk factors have been proposed:
- Retrograde Menstruation: Menstrual blood flows backward through the fallopian tubes into the pelvic cavity, allowing endometrial-like cells to implant and grow outside the uterus.
- Embryonic Cell Transformation: Hormonal factors may transform embryonic cells into endometrial-like cell implants during puberty.
- Surgical Scars: Postoperative implantation of endometrial cells during procedures such as cesarean sections or hysterectomies.
- Immune System Disorders: Anomalies in immune function may hinder the body’s ability to recognize and eliminate ectopic endometrial tissue.
- Genetics: A familial predisposition suggests a genetic component, with first-degree relatives of affected individuals having a higher risk.
Diagnosis
Diagnosing endometriosis can be challenging due to its nonspecific symptoms and overlap with other conditions. The diagnostic process may involve:
- Clinical Evaluation: Detailed medical history and pelvic examination to identify abnormalities.
- Imaging Studies: Transvaginal ultrasound and magnetic resonance imaging (MRI) can detect endometriotic cysts and deep infiltrating lesions.
- Laparoscopy: A minimally invasive surgical procedure considered the gold standard for definitive diagnosis, allowing direct visualization and biopsy of endometrial implants.
Treatment Options
Management of endometriosis is tailored to individual symptoms, disease severity, and reproductive goals:
- Medications:
- Pain Relief: Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to alleviate pain.
- Hormonal Therapies: Aim to reduce or eliminate menstruation, thus slowing endometrial tissue growth. Options include:
- Oral contraceptives
- Gonadotropin-releasing hormone (GnRH) agonists and antagonists
- Progestin therapy
- Aromatase inhibitors
- Surgical Interventions:
- Conservative Surgery: Laparoscopic excision or ablation of endometrial implants to relieve pain and improve fertility.
- Definitive Surgery: Hysterectomy with or without oophorectomy for severe cases unresponsive to other treatments, typically considered when fertility preservation is not a concern.
- Assisted Reproductive Technologies (ART): In vitro fertilization (IVF) may be recommended for those facing infertility related to endometriosis.
Impact on Fertility
Endometriosis can impair fertility through mechanisms such as:
- Distortion of pelvic anatomy
- Formation of adhesions
- Inflammation affecting ovarian and tubal function
Early diagnosis and intervention are crucial for individuals desiring pregnancy, and a multidisciplinary approach involving gynecologists and fertility specialists is often beneficial.
Living with Endometriosis
Chronic pain and other symptoms of endometriosis can significantly impact mental health, relationships, and overall quality of life. Support strategies include:
- Psychological Counseling: To address emotional challenges and develop coping mechanisms.
- Support Groups: Connecting with others facing similar experiences for shared understanding and encouragement.
- Lifestyle Modifications: Regular exercise, dietary adjustments, and stress management techniques may alleviate symptoms.