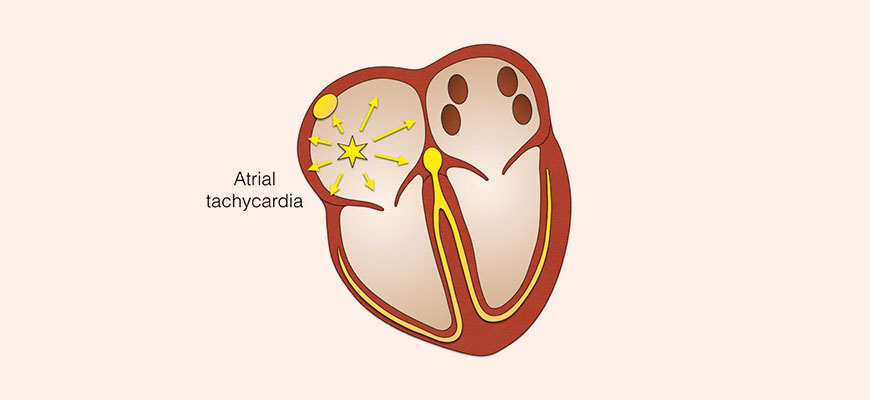
What Is Ectopic Atrial Tachycardia?
Ectopic atrial tachycardia (EAT) is a type of supraventricular tachycardia (SVT) caused by abnormal electrical impulses originating outside the sinoatrial (SA) node. Unlike normal sinus rhythm, in which the SA node controls heartbeats, EAT arises from an ectopic atrial focus, leading to a persistently elevated heart rate, often between 100 and 250 beats per minute.
EAT can occur in both pediatric and adult populations, either as an isolated condition or in association with structural heart disease. While some cases are asymptomatic, persistent or recurrent EAT can lead to complications such as tachycardia-induced cardiomyopathy.
Causes and Risk Factors
EAT is typically caused by increased automaticity, triggered activity, or reentrant circuits in the atria. Several factors may contribute to its development, including:
- Congenital abnormalities – Some individuals have ectopic foci present from birth.
- Structural heart disease – Conditions like congenital heart defects, myocarditis, and cardiomyopathies can predispose patients to EAT.
- Electrolyte imbalances – Abnormal potassium, calcium, or magnesium levels can influence atrial excitability.
- Post-surgical changes – Patients who have undergone cardiac surgeries, particularly for congenital heart defects, may develop EAT due to atrial scarring.
- Autonomic nervous system dysfunction – Increased sympathetic tone or decreased parasympathetic activity can promote ectopic activity.
- Medications and stimulants – Certain drugs, such as digitalis, catecholamines, and stimulants like caffeine or nicotine, can trigger EAT.
Symptoms of Ectopic Atrial Tachycardia
The clinical presentation of EAT varies based on heart rate, duration, and underlying cardiac function. Common symptoms include:
- Palpitations – A sensation of rapid or irregular heartbeat.
- Fatigue – Reduced cardiac efficiency may cause chronic fatigue.
- Dizziness or lightheadedness – Decreased cardiac output can lead to reduced cerebral perfusion.
- Shortness of breath (dyspnea) – Especially during exertion, due to increased oxygen demand.
- Chest discomfort – Mild to moderate chest pain may occur, particularly in prolonged episodes.
- Syncope (fainting) – Rare but possible in severe cases.
Some individuals, particularly children, may remain asymptomatic, with EAT detected incidentally on an electrocardiogram (ECG).
Diagnosis of Ectopic Atrial Tachycardia
Electrocardiography (ECG)
EAT is identified on ECG by the following characteristics:
- Abnormal P-wave morphology – Differing from sinus P-waves due to ectopic origin.
- Incessant tachycardia – Persistent atrial rates exceeding 100 bpm.
- Variable AV conduction – May present with 1:1 or varying conduction to the ventricles.
Holter Monitoring and Event Recorders
Ambulatory ECG monitoring is useful for detecting intermittent episodes or assessing tachycardia burden over 24 hours or longer.
Electrophysiological Study (EPS)
An invasive procedure used to map ectopic atrial foci and assess conduction pathways for potential ablation therapy.
Echocardiography
Evaluates structural heart disease and potential cardiomyopathy secondary to prolonged tachycardia.
Blood Tests
Assesses thyroid function, electrolyte levels, and drug-induced causes.
Treatment of Ectopic Atrial Tachycardia
Medical Therapy
Pharmacologic treatment is the first-line approach for managing EAT. Commonly used medications include:
- Beta-blockers (e.g., metoprolol, propranolol) – Reduce sympathetic activity and slow heart rate.
- Calcium channel blockers (e.g., verapamil, diltiazem) – Inhibit atrioventricular conduction and suppress ectopic activity.
- Antiarrhythmic drugs (e.g., flecainide, amiodarone, sotalol) – Used in refractory cases to maintain sinus rhythm.
Catheter Ablation
For patients with symptomatic or drug-resistant EAT, radiofrequency ablation (RFA) is a highly effective curative procedure. During RFA, targeted energy eliminates the ectopic focus, restoring normal rhythm. Success rates exceed 90% in experienced centers.
Lifestyle Modifications
Patients with EAT may benefit from:
- Avoiding triggers – Limiting caffeine, alcohol, and stimulant use.
- Managing stress – Relaxation techniques such as yoga or meditation.
- Treating underlying conditions – Addressing structural heart disease or metabolic imbalances.
Prognosis and Long-Term Outlook
The prognosis of EAT depends on its duration, frequency, and underlying heart health.
- Paroxysmal EAT – Episodes may be self-limiting, with minimal long-term effects.
- Persistent EAT – Chronic cases can lead to tachycardia-induced cardiomyopathy, which may require aggressive treatment.
- Post-ablation – Patients who undergo successful catheter ablation often achieve long-term arrhythmia control.
Early diagnosis and appropriate management significantly improve outcomes, minimizing complications associated with prolonged tachycardia.