Diverticulitis is a condition that affects the gastrointestinal (GI) tract, specifically the colon. It arises when small pouches, called diverticula, that form in the walls of the colon become inflamed or infected. The presence of diverticula without inflammation is referred to as diverticulosis. This article provides an in-depth exploration of diverticulitis, including its causes, symptoms, diagnostic methods, treatment options, and preventative measures.
What is Diverticulitis?
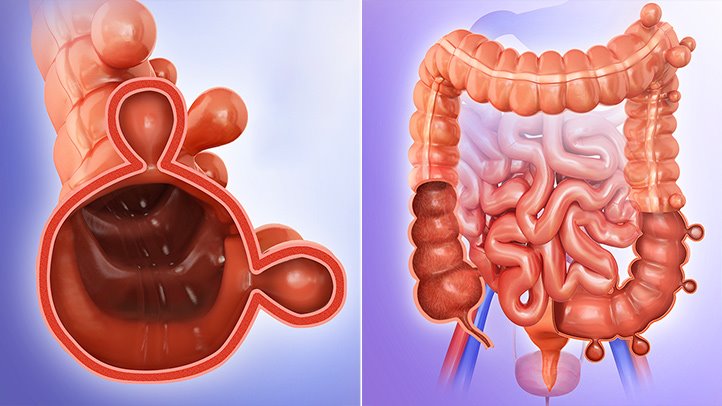
Diverticulitis occurs when diverticula, small bulging pouches that develop in the digestive tract, become inflamed or infected. Diverticula most commonly form in the lower part of the colon, called the sigmoid colon. While diverticulosis, the presence of these pouches, is relatively common, especially as individuals age, diverticulitis only develops when these pouches become problematic.
The condition ranges from mild to severe, and in some cases, can lead to serious complications like perforation, abscess formation, or sepsis.
Causes of Diverticulitis
Diverticulitis is primarily caused by the inflammation of diverticula. However, it is important to understand the factors that lead to the development of diverticula in the first place.
1. Dietary Factors
A diet low in fiber and high in processed foods is one of the primary risk factors for diverticulitis. A lack of fiber can lead to constipation and increased pressure within the colon, which in turn causes the formation of diverticula.
2. Age
The risk of developing diverticulitis increases with age. Approximately 50% of people over the age of 60 have diverticulosis, and a significant percentage may develop diverticulitis as a result.
3. Genetic Factors
Family history plays a significant role. Those with relatives who have had diverticulitis are at a higher risk of developing the condition themselves.
4. Obesity
Obesity increases the pressure within the colon, contributing to the formation of diverticula and the risk of inflammation.
5. Lack of Physical Activity
Sedentary lifestyles are linked to an increased risk of diverticulitis. Regular exercise helps regulate bowel movements and reduces colon pressure.
Symptoms of Diverticulitis
Diverticulitis can present with a range of symptoms, which may vary in severity depending on the extent of the condition.
1. Abdominal Pain
The most common symptom is pain in the lower abdomen, often on the left side. The pain can be sudden and severe, and may worsen with movement.
2. Fever
Infection of the diverticula often causes a fever, which is a sign that the body is fighting an infection.
3. Bloating and Gas
Many individuals with diverticulitis experience bloating, a sensation of fullness, or excessive gas.
4. Changes in Bowel Movements
Symptoms can include diarrhea, constipation, or alternation between the two.
5. Nausea and Vomiting
When the infection becomes more severe, nausea and vomiting may occur, often due to the body’s attempt to cope with the infection.
6. Rectal Bleeding
Although less common, bleeding from the rectum may occur if a diverticulum ruptures, though it is usually not severe.
Diagnosis of Diverticulitis
To accurately diagnose diverticulitis, healthcare providers use a variety of diagnostic tools.
1. Physical Examination
A physical exam will often reveal tenderness in the lower abdomen, particularly the left side, which is indicative of diverticulitis.
2. Blood Tests
Blood tests help identify signs of infection, such as elevated white blood cell counts and inflammation markers.
3. Imaging Tests
CT scans are the most common and effective method for diagnosing diverticulitis. A CT scan provides detailed images of the colon, revealing any inflammation or complications such as abscesses or perforations.
4. Colonoscopy
While colonoscopy is typically avoided during acute episodes of diverticulitis due to the risk of perforation, it is used after recovery to assess the presence of diverticula and rule out other conditions such as colorectal cancer.
Treatment Options for Diverticulitis
Treatment for diverticulitis depends on the severity of the condition, with approaches ranging from conservative management to surgical intervention.
1. Antibiotics
In cases of mild diverticulitis, oral antibiotics are often prescribed to treat infection. The goal is to reduce inflammation and prevent complications.
2. Dietary Changes
For mild diverticulitis, doctors often recommend a clear liquid diet initially, which can help reduce inflammation. Once symptoms improve, patients are gradually reintroduced to solid foods.
3. Hospitalization
Severe cases may require hospitalization for intravenous antibiotics, hydration, and other supportive care.
4. Surgery
If diverticulitis leads to complications such as perforation, abscesses, or fistulas, surgical intervention may be necessary. In some cases, a portion of the colon may need to be removed.
5. Pain Management
Over-the-counter pain relievers such as acetaminophen may be recommended to manage discomfort. Nonsteroidal anti-inflammatory drugs (NSAIDs) should be avoided, as they can exacerbate the condition.
Preventing Diverticulitis
While it may not be possible to completely prevent diverticulitis, several measures can significantly reduce the risk of developing the condition or prevent flare-ups in those already affected.
1. High-Fiber Diet
Eating a diet rich in fiber from fruits, vegetables, whole grains, and legumes can help prevent constipation and reduce colon pressure, lowering the risk of diverticulitis.
2. Regular Exercise
Engaging in physical activity regularly can help promote healthy digestion and bowel movements, reducing the risk of developing diverticulitis.
3. Maintaining Healthy Weight
Obesity is a risk factor for diverticulitis, so maintaining a healthy weight through diet and exercise is crucial for prevention.
4. Avoiding Smoking
Smoking has been linked to an increased risk of developing diverticulitis and other GI conditions. Quitting smoking can reduce this risk.
5. Hydration
Staying hydrated helps maintain regular bowel movements, which can reduce the strain on the colon and prevent the formation of diverticula.
Complications of Diverticulitis
If left untreated, diverticulitis can lead to several serious complications. These include:
- Perforation of the Colon: A rupture in the diverticula can lead to a perforated colon, allowing bacteria to spread into the abdominal cavity and cause peritonitis, a life-threatening infection.
- Abscess Formation: Infected diverticula can form abscesses, which may require drainage or surgical removal.
- Fistulas: Diverticulitis can cause abnormal connections between the colon and other organs, such as the bladder or vagina, leading to infections and other complications.
- Colon Obstruction: Repeated episodes of diverticulitis can cause scarring and narrowing of the colon, leading to bowel obstruction.