Disseminated blastomycosis is a systemic fungal infection caused by Blastomyces dermatitidis, a dimorphic fungus endemic to certain regions of North America. This condition arises when the primary pulmonary infection spreads hematogenously to other organs, including the skin, bones, genitourinary tract, and central nervous system. Timely diagnosis and appropriate treatment are crucial to prevent severe complications and reduce mortality.
Epidemiology
Blastomyces dermatitidis is predominantly found in the Ohio and Mississippi River valleys, the Great Lakes region, and the southeastern United States. The annual incidence in these areas ranges from less than 1 to 2 cases per 100,000 individuals. While blastomycosis can affect individuals of all ages and genders, adult males are more frequently diagnosed, possibly due to occupational and recreational exposures. Immunocompetent individuals can contract the infection; however, those with weakened immune systems may experience more severe manifestations.
Pathophysiology
Inhalation of aerosolized conidia (spores) of Blastomyces dermatitidis leads to primary pulmonary infection. Once in the lungs, the spores transform into yeast forms, which can evade phagocytosis due to their thick cell walls. The yeast can disseminate through the bloodstream and lymphatic system to various organs. The skin is the most common site of extrapulmonary involvement, followed by bones, the genitourinary system, and the central nervous system.
Clinical Manifestations
Pulmonary Blastomycosis
The initial infection often presents as a pulmonary disease, with symptoms ranging from mild respiratory issues to severe pneumonia. Common symptoms include:
- Fever
- Cough (productive or dry)
- Chest pain
- Dyspnea (shortness of breath)
- Night sweats
- Weight loss
In some cases, the infection may be asymptomatic or mimic other pulmonary conditions, leading to misdiagnosis.
Extrapulmonary Dissemination
When the infection spreads beyond the lungs, it can affect multiple organs:
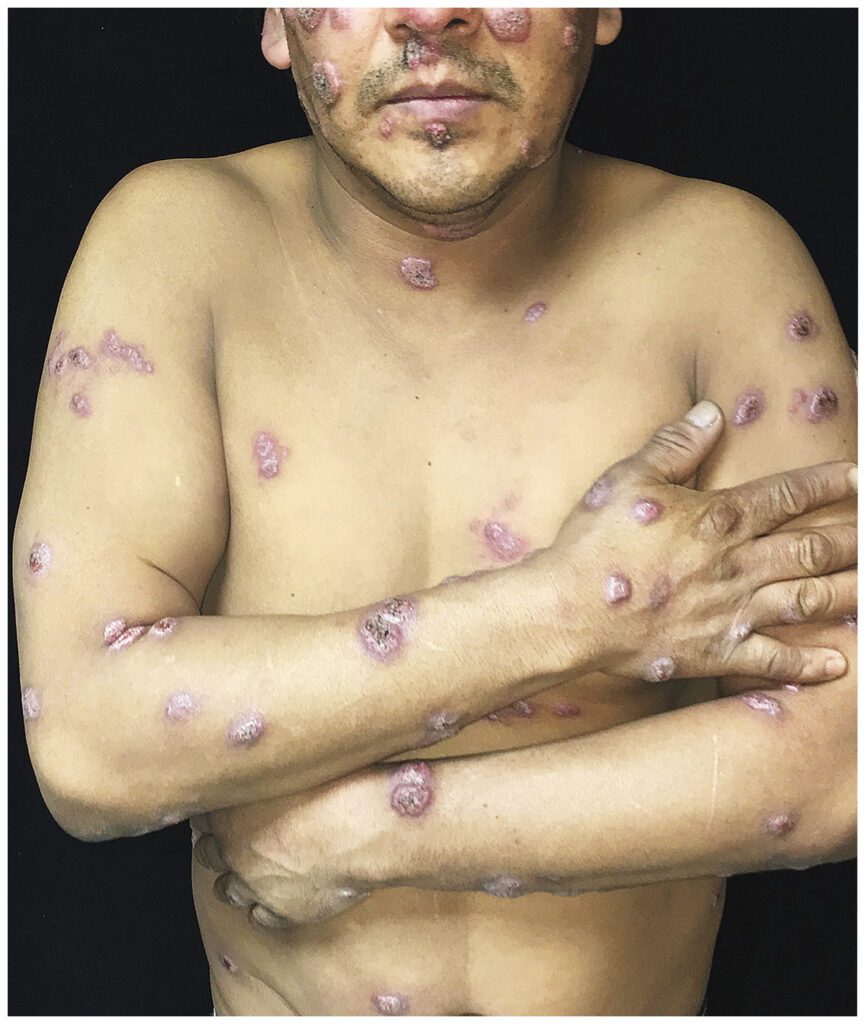
- Skin: Lesions may appear as papules, pustules, or ulcers, often on exposed areas. These can evolve into verrucous (wart-like) plaques with irregular borders.
- Bones and Joints: Osteomyelitis can develop, leading to bone pain, swelling, and lytic lesions, particularly in the vertebrae and long bones.
- Genitourinary System: In men, prostatitis and epididymitis are common, presenting with symptoms like perineal discomfort and scrotal swelling. Women may experience endometritis or tubo-ovarian abscesses.
- Central Nervous System: Though less common, the infection can lead to meningitis, brain abscesses, or epidural abscesses, presenting with headaches, altered mental status, and neurological deficits.
Diagnosis
Accurate diagnosis requires a high index of suspicion, especially in endemic areas. Diagnostic approaches include:
- Microscopic Examination: Visualization of the characteristic broad-based budding yeast in clinical specimens (e.g., sputum, tissue biopsies) using stains like potassium hydroxide (KOH) preparation or silver stains.
- Culture: Definitive diagnosis can be achieved by culturing the organism from clinical samples, though this may take several weeks.
- Antigen Detection: Enzyme immunoassays (EIA) can detect Blastomyces antigens in urine, blood, or other body fluids, offering a more rapid diagnosis. However, cross-reactivity with other fungal infections may occur.
- Imaging: Chest radiographs or CT scans may reveal pulmonary infiltrates, masses, or nodules, but these findings are non-specific.
Treatment
The choice of antifungal therapy depends on the severity of the disease and the patient’s immune status:
- Mild to Moderate Disease: Itraconazole is the preferred oral antifungal agent, administered for 6 to 12 months.
- Severe or Life-Threatening Disease: Initial treatment with intravenous amphotericin B is recommended until clinical improvement is observed, followed by a transition to oral itraconazole for a total treatment duration of at least 12 months.
- Central Nervous System Involvement: Liposomal amphotericin B is preferred due to better central nervous system penetration.
Regular monitoring for drug toxicity and therapeutic response is essential throughout the treatment course.