Diffuse proliferative lupus nephritis (DPLN) represents a severe renal manifestation of systemic lupus erythematosus (SLE). Characterized by widespread inflammation and proliferation within the glomeruli, DPLN significantly impacts renal function and patient prognosis. A thorough understanding of its pathophysiology, clinical presentation, diagnostic criteria, and treatment options is essential for effective management.
Pathophysiology of Diffuse Proliferative Lupus Nephritis
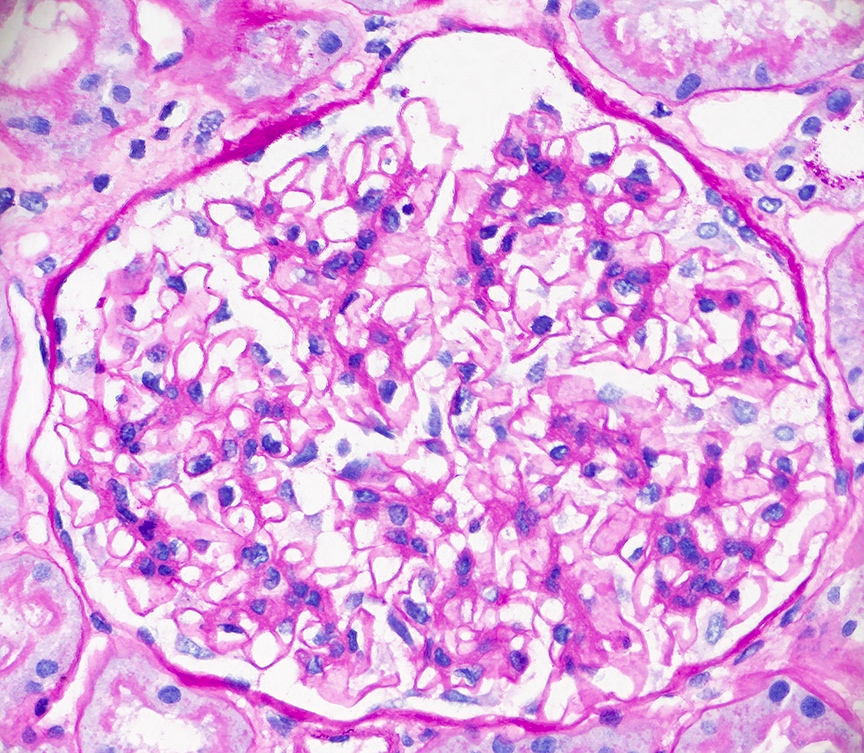
DPLN is classified as Class IV lupus nephritis under the World Health Organization (WHO) and International Society of Nephrology/Renal Pathology Society (ISN/RPS) systems. This classification denotes involvement of more than 50% of glomeruli with endocapillary proliferation and immune complex deposition, primarily in subendothelial spaces. The immune complexes, composed of autoantibodies such as anti-double-stranded DNA (anti-dsDNA), deposit in the glomeruli, triggering complement activation and an inflammatory cascade that leads to glomerular injury and sclerosis.
Clinical Manifestations
Patients with DPLN may present with a spectrum of renal and systemic symptoms, including:
- Proteinuria: Often in the nephrotic range, indicating significant glomerular damage.
- Hematuria: Microscopic or gross blood in the urine due to glomerular inflammation.
- Hypertension: Elevated blood pressure resulting from renal impairment.
- Edema: Swelling in extremities and face due to hypoalbuminemia from protein loss.
- Elevated Serum Creatinine: Reflecting decreased glomerular filtration rate and renal function.
Systemic symptoms of SLE, such as arthralgia, malar rash, and fatigue, may also be present.
Diagnostic Criteria
Accurate diagnosis of DPLN involves a combination of laboratory assessments and renal biopsy:
- Laboratory Tests:
- Urinalysis: Detection of proteinuria, hematuria, and cellular casts.
- Serology: Elevated anti-dsDNA antibodies and decreased complement levels (C3, C4) are indicative of active disease.
- Renal Function Tests: Elevated serum creatinine and blood urea nitrogen levels.
- Renal Biopsy: Essential for definitive diagnosis, biopsy findings in DPLN include:
- Light Microscopy: Diffuse endocapillary proliferation with or without crescents.
- Immunofluorescence: Granular deposits of immunoglobulins (IgG, IgA, IgM) and complement components (C1q, C3) along the glomerular basement membrane and mesangium.
- Electron Microscopy: Subendothelial and mesangial electron-dense deposits.
Treatment Strategies
Management of DPLN requires a multifaceted approach aimed at inducing remission, preventing relapse, and preserving renal function:
- Induction Therapy: Typically involves high-dose corticosteroids combined with immunosuppressive agents such as cyclophosphamide or mycophenolate mofetil (MMF). Recent studies suggest MMF may offer a favorable safety profile compared to cyclophosphamide.
- Maintenance Therapy: Following induction, maintenance therapy with lower doses of immunosuppressants (MMF or azathioprine) is employed to sustain remission and prevent relapse.
- Adjunctive Therapies:
- Hydroxychloroquine: Recommended for all SLE patients unless contraindicated, due to its immunomodulatory effects and potential to reduce flares.
- Angiotensin-Converting Enzyme Inhibitors (ACEIs) or Angiotensin II Receptor Blockers (ARBs): Utilized to manage hypertension and reduce proteinuria.
- Lifestyle Modifications: Dietary sodium restriction, smoking cessation, and regular monitoring of renal function are essential components of comprehensive care.
Prognosis
The prognosis of DPLN has improved with advancements in immunosuppressive therapy. However, it remains a significant cause of morbidity in SLE patients. Factors associated with a poorer prognosis include:
- Delayed Diagnosis: Emphasizing the importance of early detection and intervention.
- Poor Treatment Adherence: Highlighting the need for patient education and support.
- Presence of Chronic Lesions on Biopsy: Such as glomerular sclerosis and interstitial fibrosis, which are indicative of irreversible damage.
Regular follow-up with a multidisciplinary team is crucial to monitor disease activity, manage complications, and adjust therapy as needed.