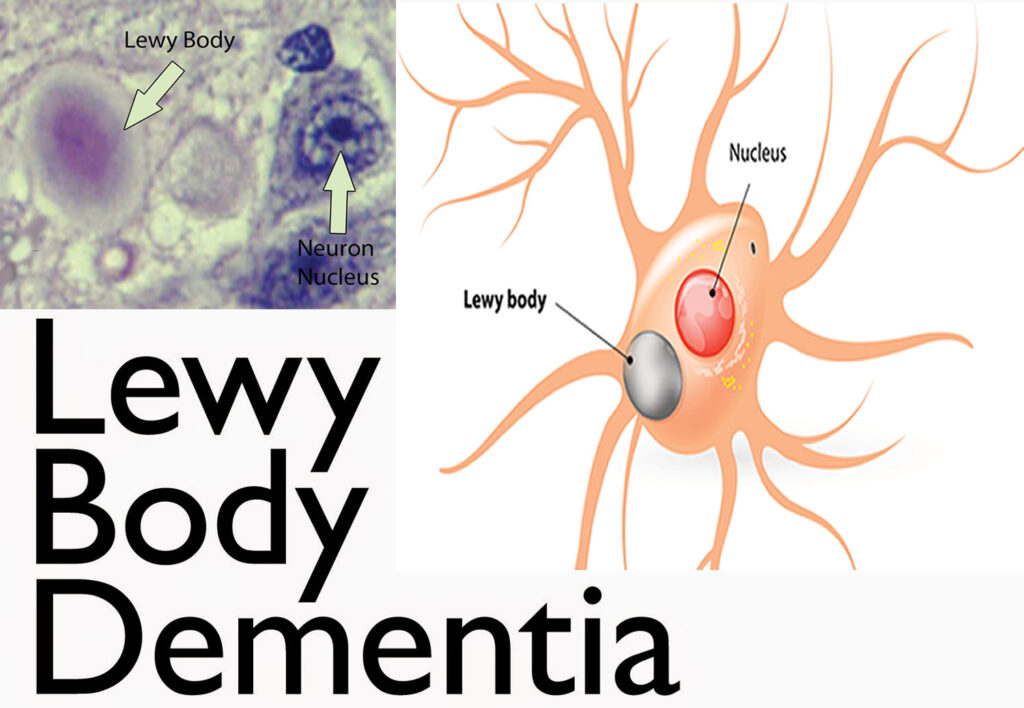
Diffuse Lewy body disease, also known as dementia with Lewy bodies (DLB), is a progressive neurodegenerative disorder characterized by the abnormal accumulation of alpha-synuclein proteins in the brain. These protein deposits, termed Lewy bodies, disrupt normal brain function, leading to a decline in cognitive, motor, and autonomic functions.
Epidemiology
DLB is recognized as the second most common form of degenerative dementia following Alzheimer’s disease. It accounts for approximately 10% to 15% of all dementia cases. The condition predominantly affects individuals over the age of 65, with a slight male predominance.
Clinical Features
The clinical presentation of DLB is diverse, encompassing a range of cognitive, motor, and behavioral symptoms.
Cognitive Impairment
Patients often experience:
- Fluctuating Attention and Alertness: Episodes of confusion or reduced awareness that can vary significantly throughout the day.
- Visuospatial Difficulties: Challenges in spatial orientation and depth perception, leading to difficulties in navigation and recognizing objects.
- Memory Impairment: While less pronounced in the early stages compared to Alzheimer’s disease, memory deficits become more evident as the disease progresses.
Visual Hallucinations
A hallmark of DLB, these hallucinations are typically vivid and detailed, often involving people or animals. Patients may recognize these perceptions as false, especially in the early stages.
Parkinsonism
Motor symptoms resembling Parkinson’s disease are common and include:
- Bradykinesia: Slowness of movement.
- Muscular Rigidity: Increased muscle tone leading to stiffness.
- Resting Tremor: Less common in DLB compared to Parkinson’s disease.
- Postural Instability: Balance issues leading to frequent falls.
Rapid Eye Movement (REM) Sleep Behavior Disorder
This manifests as:
- Vivid Dreams: Often accompanied by vocalizations and movements.
- Dream Enactment Behaviors: Physical acting out of dreams, which can result in injury.
Autonomic Dysfunction
Patients may exhibit:
- Orthostatic Hypotension: A significant drop in blood pressure upon standing, causing dizziness or fainting.
- Urinary Incontinence: Loss of bladder control.
- Constipation: Due to slowed gastrointestinal motility.
Pathophysiology
The defining feature of DLB is the widespread presence of Lewy bodies—abnormal aggregates of alpha-synuclein protein—within neurons. These inclusions are predominantly found in:
- Cerebral Cortex: Affecting cognitive functions.
- Substantia Nigra: Leading to motor symptoms due to dopaminergic neuron loss.
- Autonomic Nervous System: Resulting in autonomic dysfunctions.
The exact mechanism by which alpha-synuclein aggregation leads to neuronal death remains under investigation. However, it’s believed that these aggregates disrupt cellular processes, leading to neurodegeneration.
Diagnostic Criteria
The diagnosis of DLB is primarily clinical, supported by specific criteria:
- Core Clinical Features: Presence of at least two of the following:
- Fluctuating cognition with pronounced variations in attention and alertness.
- Recurrent visual hallucinations that are well-formed and detailed.
- Spontaneous motor features of parkinsonism.
- REM sleep behavior disorder.
- Supportive Clinical Features: Including severe sensitivity to antipsychotics, repeated falls, syncope, transient unexplained loss of consciousness, severe autonomic dysfunction, and hypersomnia.
- Indicative Biomarkers: Such as reduced dopamine transporter uptake in basal ganglia demonstrated by SPECT or PET imaging.
Differential Diagnosis
DLB shares overlapping features with several other neurodegenerative disorders:
- Alzheimer’s Disease: Both may present with cognitive decline, but visual hallucinations and parkinsonism are more suggestive of DLB.
- Parkinson’s Disease Dementia: Differentiation is based on the temporal sequence of symptoms; if dementia occurs before or within one year of parkinsonism, DLB is diagnosed. If dementia develops after a longer duration of established Parkinson’s disease, Parkinson’s disease dementia is considered.
- Vascular Dementia: Characterized by a stepwise decline in cognitive function due to cerebrovascular events, which can be distinguished through neuroimaging.
Management
Currently, there is no cure for DLB, and treatment focuses on symptom management:
- Cognitive Symptoms: Cholinesterase inhibitors, such as rivastigmine and donepezil, have shown modest benefits in improving cognitive function and reducing hallucinations.
- Motor Symptoms: Levodopa may be used cautiously to alleviate parkinsonism, though patients often exhibit limited response and may experience exacerbated hallucinations.
- Behavioral Symptoms: Non-pharmacological approaches are preferred. If medications are necessary, atypical antipsychotics like quetiapine may be considered at the lowest effective dose due to the risk of severe neuroleptic sensitivity.
- Sleep Disturbances: Melatonin is often the first-line treatment for REM sleep behavior disorder. Clonazepam may be considered if melatonin is ineffective.
Prognosis
DLB is a progressive disorder with a variable course. The average survival time after diagnosis ranges from 5 to 8 years. Disease progression is marked by increasing cognitive and motor impairment, leading to significant functional decline.