Diffuse Large B-Cell Lymphoma (DLBCL) is the most common type of non-Hodgkin lymphoma (NHL), accounting for approximately 30-40% of all NHL cases worldwide. This aggressive malignancy originates in B lymphocytes, a crucial component of the immune system. While it can occur at any age, it is more prevalent in older adults, with a median diagnosis age of around 65 years.
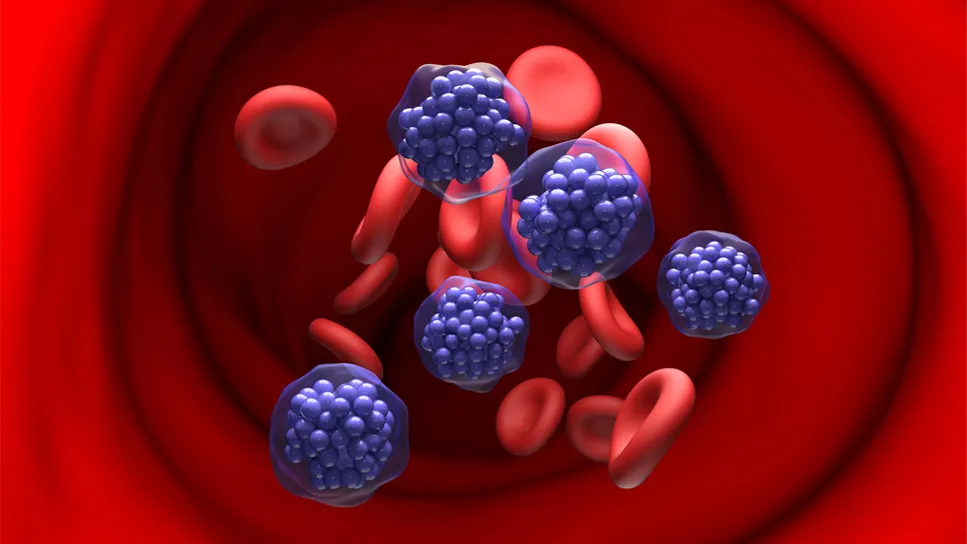
Understanding DLBCL is essential for early detection, precise diagnosis, and effective treatment strategies. This guide explores its subtypes, symptoms, risk factors, diagnostic procedures, and available treatments.
Subtypes of DLBCL
DLBCL is a heterogeneous disease with multiple subtypes, each differing in prognosis and response to treatment. The primary subtypes include:
1. Germinal Center B-Cell-Like (GCB) DLBCL
- Originates from B cells in the germinal center of lymph nodes
- Generally associated with a better prognosis
- More responsive to standard immunochemotherapy
2. Activated B-Cell-Like (ABC) DLBCL
- Develops from activated B cells outside the germinal center
- Exhibits a more aggressive disease course
- Less responsive to standard treatments but may benefit from novel targeted therapies
3. Primary Mediastinal B-Cell Lymphoma (PMBCL)
- Affects younger individuals, particularly females
- Arises in the thymic region of the mediastinum
- Often presents as a large mass in the chest
4. Double-Hit and Triple-Hit Lymphomas
- Characterized by genetic alterations in MYC, BCL2, and/or BCL6
- Highly aggressive and challenging to treat
5. T-Cell/Histiocyte-Rich Large B-Cell Lymphoma
- A rare subtype with extensive inflammatory cell infiltration
- Often involves the spleen, liver, and bone marrow
Symptoms of DLBCL
DLBCL can manifest with a wide range of symptoms, often depending on the location and extent of the disease. Common symptoms include:
- Painless swelling of lymph nodes (neck, armpits, groin)
- Fever, night sweats, and unexplained weight loss (B symptoms)
- Fatigue and weakness
- Shortness of breath or chest pain (if mediastinal involvement)
- Abdominal pain or bloating (if gastrointestinal involvement)
Risk Factors
While the exact cause of DLBCL remains unclear, several risk factors have been identified:
- Age: More common in individuals over 60 years old
- Gender: Slightly more frequent in males
- Immunosuppression: Higher risk in individuals with HIV, organ transplants, or autoimmune diseases
- Genetic Mutations: Alterations in MYC, BCL2, and BCL6 genes contribute to aggressive forms
- Chronic Infections: Epstein-Barr virus (EBV) and Helicobacter pylori have been linked to certain cases
Diagnosis
A thorough diagnostic approach is critical for accurate classification and treatment planning. Key diagnostic methods include:
1. Physical Examination
- Assessment of lymph node swelling, spleen, and liver enlargement
2. Imaging Studies
- CT scan, PET scan, or MRI: Determines disease spread and staging
3. Biopsy
- Lymph Node Biopsy: Gold standard for DLBCL diagnosis
- Bone Marrow Biopsy: Evaluates bone marrow involvement
4. Laboratory Tests
- Blood tests: Evaluate lactate dehydrogenase (LDH) levels and complete blood count (CBC)
- Flow Cytometry: Identifies specific cell markers
5. Genetic and Molecular Testing
- Determines the presence of MYC, BCL2, and BCL6 gene mutations
- Essential for identifying double-hit and triple-hit lymphomas
Staging of DLBCL
DLBCL is staged using the Ann Arbor Staging System:
Treatment Options
The treatment strategy for DLBCL depends on the disease stage, subtype, and patient-specific factors.
1. Immunochemotherapy
- R-CHOP (Rituximab, Cyclophosphamide, Doxorubicin, Vincristine, Prednisone): Standard first-line therapy
- DA-EPOCH-R: Used for high-risk subtypes
2. Targeted Therapy
- Polatuzumab vedotin: Used for relapsed or refractory cases
- Bruton’s Tyrosine Kinase (BTK) Inhibitors: Effective in ABC-DLBCL
3. Radiation Therapy
- Used for localized disease or bulky tumors
4. Stem Cell Transplantation
- Autologous Stem Cell Transplant (ASCT): Considered for relapsed patients
- CAR-T Cell Therapy: Promising option for refractory DLBCL
Prognosis and Survival Rates
DLBCL prognosis varies depending on age, disease stage, and treatment response. The International Prognostic Index (IPI) is commonly used for risk stratification:
- Low-Risk (0-1 Factors): >80% 5-year survival
- Intermediate-Risk (2-3 Factors): 50-70% 5-year survival
- High-Risk (4-5 Factors): <50% 5-year survival