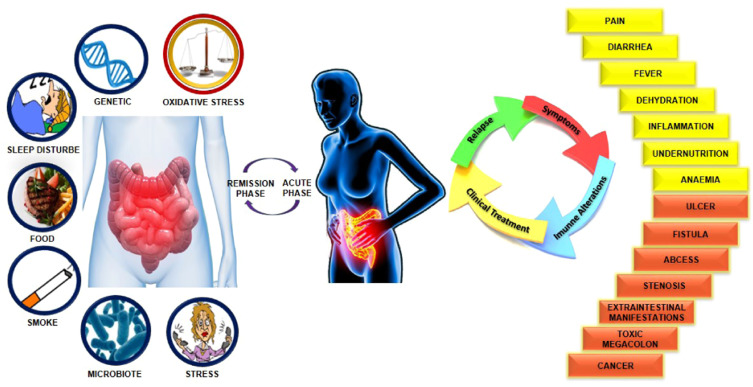
Inflammatory Bowel Disease (IBD) encompasses chronic inflammatory conditions of the gastrointestinal tract, primarily Crohn’s disease and ulcerative colitis. A prevalent and distressing symptom of IBD is diarrhea, which significantly impairs patients’ quality of life. This article delves into the intricate relationship between IBD and diarrhea, exploring its causes, manifestations, and management strategies.
Understanding Inflammatory Bowel Disease
IBD is characterized by prolonged inflammation of the digestive tract, leading to various gastrointestinal symptoms. The two primary forms are:
- Crohn’s Disease: This condition can affect any part of the gastrointestinal tract, from the mouth to the anus, and often involves the deeper layers of the bowel wall.
- Ulcerative Colitis: This form is limited to the colon and rectum, affecting only the innermost lining of the colon.
Both conditions result in chronic inflammation, which disrupts the normal function of the digestive system.
Causes of Diarrhea in IBD
Diarrhea in IBD patients arises from multiple factors:
- Inflammation: The inflamed intestinal lining impairs fluid absorption, leading to loose stools.
- Bile Acid Malabsorption: Particularly in Crohn’s disease affecting the ileum, the reduced reabsorption of bile acids can cause diarrhea.
- Medications: Certain IBD treatments, such as antibiotics and some anti-inflammatory drugs, may induce diarrhea as a side effect.
- Infections: IBD patients are susceptible to intestinal infections, which can exacerbate diarrhea.
- Dietary Factors: Food intolerances or sensitivities may trigger or worsen diarrhea symptoms.
Symptoms Associated with IBD-Related Diarrhea
Beyond frequent loose stools, patients may experience:
- Abdominal Pain and Cramping: Due to intestinal inflammation and spasms.
- Urgency: A sudden, compelling need to defecate.
- Rectal Bleeding: Presence of blood in the stool, more common in ulcerative colitis.
- Fatigue: Resulting from nutrient malabsorption and chronic inflammation.
- Weight Loss: Due to decreased appetite and poor nutrient absorption.
Diagnostic Approaches
Accurate diagnosis is crucial for effective management. Diagnostic methods include:
- Colonoscopy: Allows direct visualization and biopsy of the colon to assess inflammation extent.
- Stool Tests: To rule out infections and assess inflammation markers.
- Blood Tests: To detect anemia and evaluate overall health status.
- Imaging Studies: Techniques like CT or MRI scans help visualize the small intestine and identify complications.
Management Strategies
Managing diarrhea in IBD involves a multifaceted approach:
- Medication: Depending on disease severity and location, treatments may include:
- Aminosalicylates: Reduce inflammation in the intestinal lining.
- Corticosteroids: Used for short-term control of acute flare-ups.
- Immunomodulators: Suppress the immune response to decrease inflammation.
- Biologic Therapies: Target specific components of the immune system to control inflammation.
- Dietary Modifications: Identifying and avoiding trigger foods, maintaining a balanced diet, and considering low-residue or low-fiber diets during flare-ups can be beneficial.
- Hydration: Ensuring adequate fluid intake to prevent dehydration from frequent bowel movements.
- Probiotics: May help restore healthy gut flora balance, potentially reducing diarrhea episodes.
- Surgery: In cases where medical management is ineffective, surgical interventions may be necessary to remove affected bowel segments.
Potential Complications
If not adequately managed, diarrhea in IBD can lead to:
- Dehydration: Due to significant fluid loss.
- Electrolyte Imbalances: Loss of essential minerals can disrupt bodily functions.
- Malnutrition: Chronic diarrhea can impair nutrient absorption, leading to deficiencies.
- Anemia: Chronic blood loss may result in reduced red blood cell counts.

