Diagnostic test for growth hormone secretion plays a vital role in metabolism, growth, and glucose regulation. However, in individuals with severe insulin resistance, the physiological feedback mechanisms between insulin and GH are significantly altered, complicating the assessment of GH secretion. Traditional diagnostic tests may yield misleading results, requiring tailored approaches to accurately evaluate GH function in these patients.
This article explores the best diagnostic strategies for assessing GH secretion in the presence of severe insulin resistance, detailing the mechanisms, challenges, and clinical implications of different testing methods.
The Role of Growth Hormone in Metabolism and Insulin Sensitivity
GH influences glucose metabolism by antagonizing insulin action, promoting gluconeogenesis, and reducing peripheral glucose uptake. Under normal conditions, insulin enhances hepatic GH receptor expression, regulating GH sensitivity. However, in cases of severe insulin resistance—such as those associated with lipodystrophy, genetic insulin receptor mutations (e.g., Donohue syndrome, Rabson-Mendenhall syndrome), or metabolic syndrome—GH secretion and function can be significantly disrupted.
Effects of Severe Insulin Resistance on GH Secretion
- Disrupted GH Feedback Mechanism: Insulin normally inhibits GH secretion through somatostatin activation; severe insulin resistance disrupts this pathway.
- Altered GH Pulsatility: GH is secreted in a pulsatile manner; insulin-resistant states may modify these patterns.
- Potential GH Hypersecretion or Deficiency: Some patients with insulin resistance may exhibit paradoxical GH elevation, while others may have functional GH deficiency due to receptor-level disturbances.
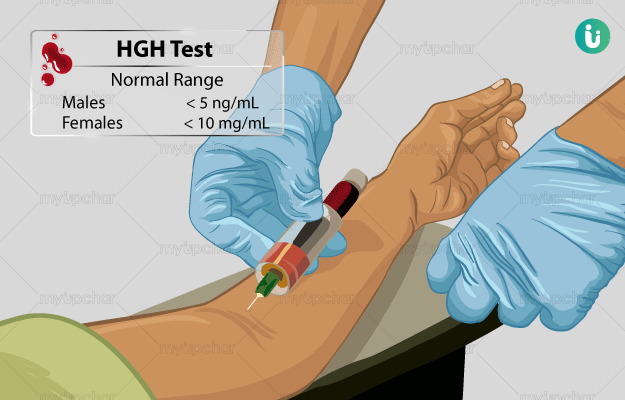
Diagnostic Tests for Growth Hormone Secretion
1. Insulin Tolerance Test (ITT) – Gold Standard with Limitations
The insulin tolerance test (ITT) is the most reliable method for assessing GH secretion by inducing hypoglycemia, a potent GH stimulus. However, in severe insulin resistance:
- Hypoglycemia may be difficult to achieve, reducing test accuracy.
- Patients with extreme insulin resistance may require impractically high insulin doses.
- The test carries risks, especially in patients with cardiovascular conditions.
2. Glucagon Stimulation Test (GST) – Alternative in Insulin-Resistant Patients
Glucagon stimulates GH secretion via transient hypoglycemia and catecholamine release. This test is preferred in patients where ITT is contraindicated, though:
- GH responses may be blunted in metabolic disorders.
- The prolonged testing duration (3–4 hours) can be a limitation.
3. GHRH-Arginine Stimulation Test – Evaluating Pituitary GH Reserve
Combining growth hormone-releasing hormone (GHRH) with arginine enhances GH release by suppressing somatostatin. This test is beneficial for:
- Differentiating pituitary versus hypothalamic GH dysfunction.
- Assessing GH reserve in cases with unclear ITT/GST results.
4. Clonidine and L-DOPA Tests – Limited Use in Insulin Resistance
Clonidine (an α2-adrenergic agonist) and L-DOPA stimulate GH release through central pathways but have variable reliability in severe insulin resistance. Their diagnostic value is lower compared to ITT and GST.
5. Oral Glucose Tolerance Test (OGTT) – Useful in GH Excess Disorders
Though primarily used to diagnose acromegaly, the OGTT can help distinguish abnormal GH suppression patterns in insulin-resistant patients suspected of GH excess rather than deficiency.
Challenges in GH Testing for Insulin-Resistant Patients
- Increased Basal GH Levels: Some insulin-resistant conditions present with paradoxically high GH, confounding test interpretations.
- Blunted GH Responses: Chronic hyperinsulinemia may desensitize GH-releasing mechanisms.
- Coexisting Endocrine Disorders: Thyroid dysfunction, adrenal abnormalities, or leptin resistance can interfere with GH test results.
Approach to Test Interpretation:
| Test | Expected GH Response in Normal Patients | GH Response in Severe Insulin Resistance |
|---|---|---|
| ITT | Significant GH rise (>5 µg/L) | Blunted or exaggerated response |
| GST | Moderate GH rise | Variable response |
| GHRH-Arginine | Strong GH increase | May differentiate pituitary vs. receptor defects |
| Clonidine/L-DOPA | GH elevation | Often unreliable |
| OGTT | GH suppression | Possible GH paradox |
Clinical Implications and Next Steps
Proper interpretation of GH secretion tests is crucial for diagnosing GH deficiency or excess in insulin-resistant individuals. Treatment decisions—such as GH replacement therapy or metabolic interventions—should be guided by a comprehensive endocrine evaluation.
Key Takeaways:
- The insulin tolerance test (ITT) remains the gold standard but has limitations in severe insulin resistance.
- Glucagon stimulation and GHRH-arginine tests serve as safer alternatives.
- OGTT can help assess GH excess in insulin-resistant states.
- Test interpretation requires caution, considering metabolic and endocrine confounders.