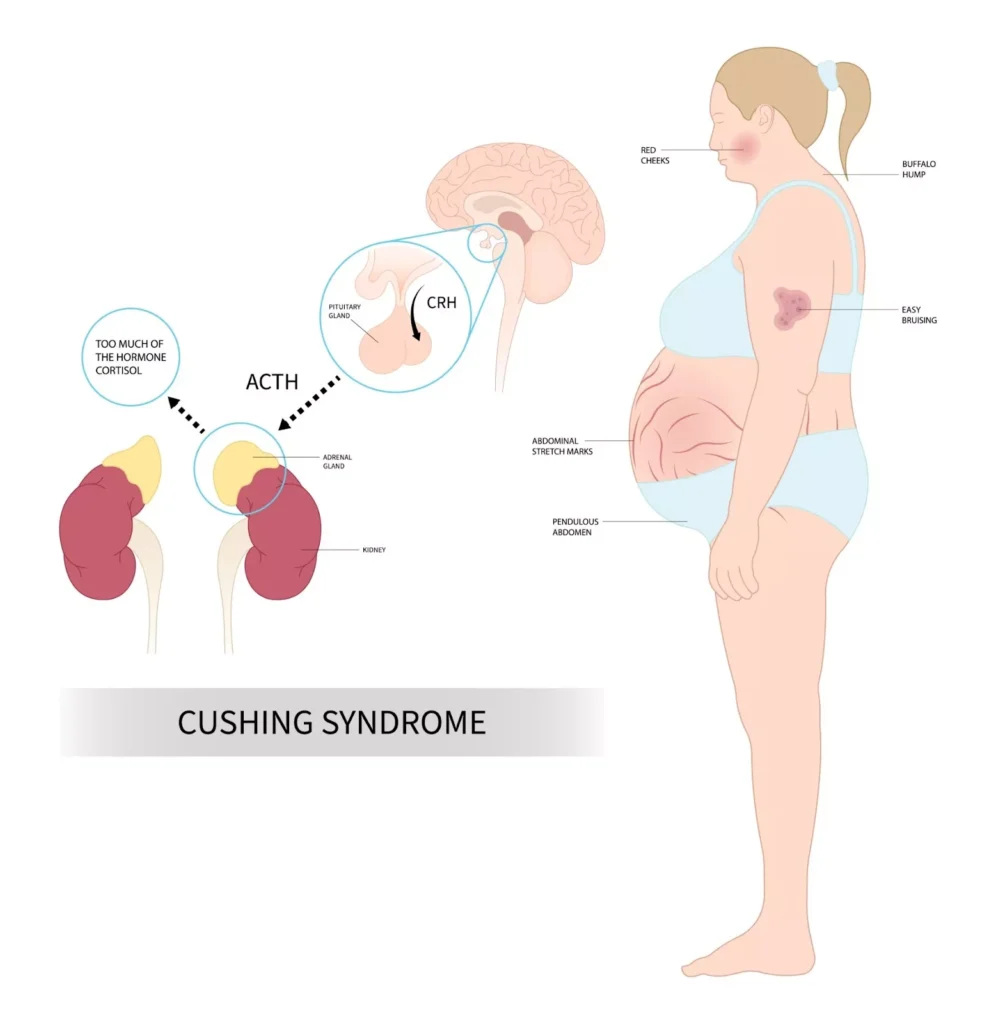
Diagnostic test for cushing’s syndrome results from prolonged exposure to excessive cortisol, leading to significant metabolic consequences. When coupled with severe insulin resistance, the diagnostic process becomes complex due to overlapping clinical features and altered hormonal responses. A meticulous approach involving multiple biochemical and imaging tests is crucial for an accurate diagnosis.
Screening Tests for Hypercortisolism
The first step in diagnosing Cushing’s syndrome is confirming endogenous hypercortisolism through screening tests.
1. 24-Hour Urinary Free Cortisol (UFC) Test
- Measures the amount of unbound cortisol excreted in urine over 24 hours.
- Elevated UFC levels suggest hypercortisolism.
- Multiple collections are recommended due to cortisol secretion variability.
2. Late-Night Salivary Cortisol Test
- Cortisol levels should normally decline in the evening.
- Elevated late-night salivary cortisol suggests loss of diurnal rhythm, a hallmark of Cushing’s syndrome.
- Non-invasive and useful for outpatient evaluation.
3. Overnight 1-mg Dexamethasone Suppression Test (DST)
- Involves oral administration of 1 mg dexamethasone at night, followed by serum cortisol measurement the next morning.
- A cortisol level >1.8 µg/dL (50 nmol/L) suggests CS.
- Requires careful interpretation due to potential influence from medications, obesity, and comorbid conditions.
Challenges in Patients with Severe Insulin Resistance
Severe insulin resistance complicates the diagnostic process due to metabolic overlap and altered cortisol metabolism.
- Metabolic Overlap: Both CS and severe insulin resistance exhibit central obesity, hypertension, and glucose intolerance.
- Altered Cortisol Metabolism: Insulin resistance affects cortisol clearance and feedback mechanisms.
- Medication Interference: Insulin-sensitizing agents can influence cortisol levels and test accuracy.
Differential Diagnosis of Hypercortisolism
Once hypercortisolism is confirmed, determining the underlying cause is essential.
1. Plasma Adrenocorticotropic Hormone (ACTH) Measurement
- Low ACTH (<5 pg/mL): Suggests an adrenal source (adrenal adenoma or carcinoma).
- Normal or Elevated ACTH (>10 pg/mL): Indicates ACTH-dependent CS (pituitary adenoma or ectopic ACTH secretion).
2. High-Dose Dexamethasone Suppression Test
- Differentiates pituitary-dependent Cushing’s disease from ectopic ACTH syndrome.
- In Cushing’s disease, high-dose dexamethasone suppresses cortisol production, while ectopic ACTH secretion remains unaffected.
3. Imaging Studies
- Pituitary MRI: Identifies pituitary adenomas in ACTH-dependent cases.
- Adrenal CT Scan: Detects adrenal tumors or hyperplasia in ACTH-independent CS.
4. Inferior Petrosal Sinus Sampling (IPSS)
- Used when imaging is inconclusive.
- Compares ACTH levels in the inferior petrosal sinuses and peripheral circulation.
- A central-to-peripheral ACTH ratio >2 at baseline or >3 after corticotropin-releasing hormone (CRH) stimulation confirms pituitary origin.
Advanced Evaluations in Severe Insulin Resistance
Given the complexities of diagnosing CS in insulin-resistant patients, additional tests may be required.
- Insulin Tolerance Test (ITT): Assesses hypothalamic-pituitary-adrenal axis function but carries risks in patients with severe insulin resistance.
- Salivary Testing: Non-invasive method for assessing circadian cortisol variation, useful in challenging diagnostic cases.