Diagnostic test for asthma in patients with severe insulin resistance (IR) necessitates a nuanced approach, considering the intricate relationship between metabolic dysfunction and respiratory health. Recent studies have illuminated the impact of IR on lung function, underscoring the importance of tailored diagnostic strategies.
Understanding the Interplay Between Asthma and Insulin Resistance
Insulin resistance, a hallmark of metabolic syndrome, has been implicated in respiratory impairments. Research indicates that IR is prevalent among asthma patients and is associated with decreased lung function and suboptimal responses to standard asthma treatments. This association persists independently of obesity, suggesting a direct link between metabolic and respiratory systems.
Comprehensive Diagnostic Evaluation
- Detailed Medical History and Physical Examination
- Medical History: Elicit information on respiratory symptoms, their frequency, and potential triggers. Inquire about a history of allergies, eczema, or familial predisposition to asthma and metabolic disorders.
- Physical Examination: Conduct a thorough examination focusing on respiratory and cardiovascular systems. Assess for signs of obesity and other metabolic syndrome components.
- Pulmonary Function Tests (PFTs)
- Spirometry: Measures forced vital capacity (FVC) and forced expiratory volume in one second (FEV₁). A reduced FEV₁/FVC ratio may indicate airway obstruction characteristic of asthma.
- Bronchodilator Reversibility Testing: Administer a bronchodilator and repeat spirometry to assess for reversible airway obstruction, a hallmark of asthma.
- Assessment of Airway Inflammation
- Fractional Exhaled Nitric Oxide (FeNO): Elevated FeNO levels can indicate eosinophilic airway inflammation, commonly seen in asthma. However, patients with IR may exhibit lower FeNO levels, reflecting a non-eosinophilic phenotype.
- Metabolic Evaluation
- Homeostatic Model Assessment of Insulin Resistance (HOMA-IR): Calculate HOMA-IR to quantify insulin resistance levels. Elevated HOMA-IR has been associated with impaired lung function in asthma patients.
- Lipid Profile and Glucose Levels: Assess for dyslipidemia and hyperglycemia, components of metabolic syndrome that may influence asthma severity.
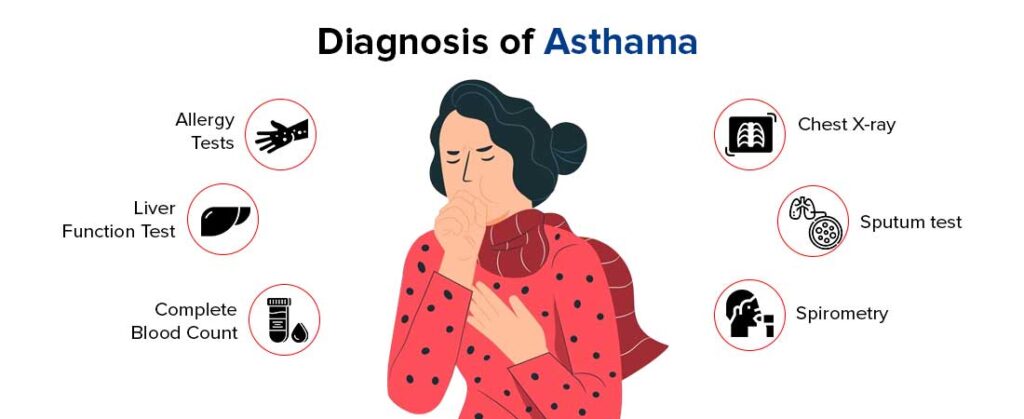
- Allergy Testing
- Skin Prick Tests or Serum IgE Levels: Identify atopic triggers that could exacerbate asthma symptoms.
- Imaging Studies
- Chest Radiography or High-Resolution Computed Tomography (HRCT): Rule out alternative diagnoses or comorbid conditions that may mimic or complicate asthma.
Integrating Diagnostic Findings
The diagnostic process should integrate pulmonary function results, inflammatory markers, and metabolic assessments. Recognizing that patients with severe IR may present with a distinct asthma phenotype—characterized by non-eosinophilic inflammation and reduced responsiveness to standard therapies—is crucial for accurate diagnosis and management.
Diagnosing asthma in the context of severe insulin resistance requires a comprehensive and multidisciplinary approach. By considering the complex interplay between metabolic and respiratory health, clinicians can develop more effective, individualized management plans for this unique patient population.