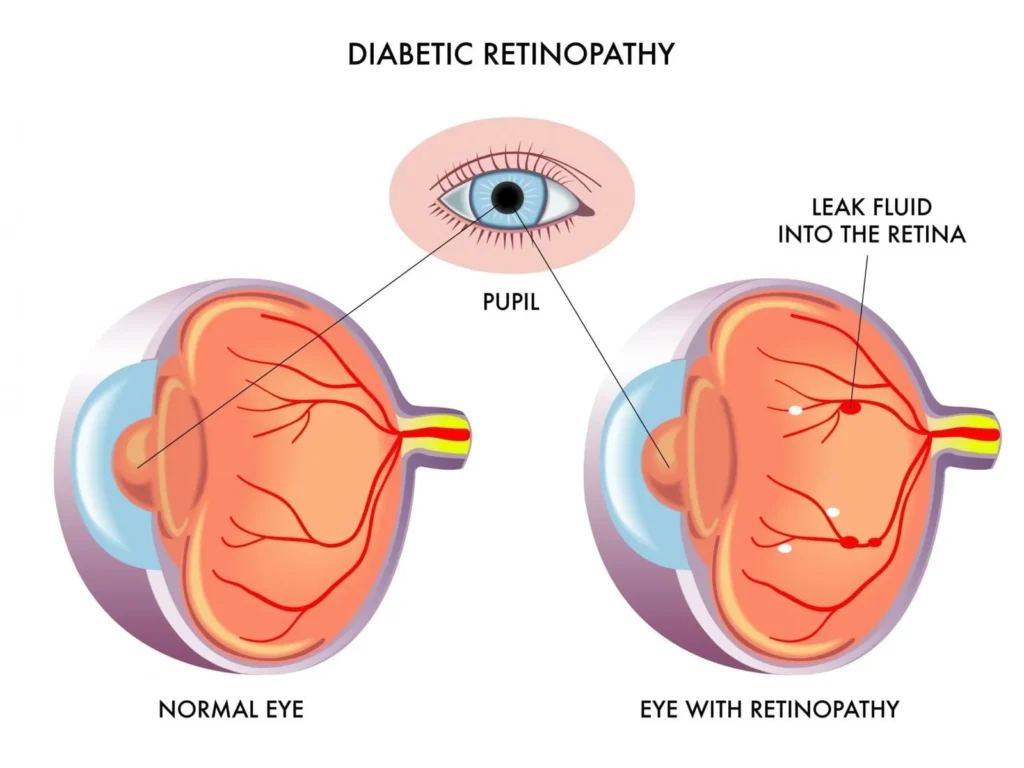
Diabetic retinopathy (DR) is a serious complication of diabetes that affects the retina, leading to vision impairment and potential blindness. When coupled with severe insulin resistance (SIR), the condition becomes even more complex, requiring aggressive management to prevent irreversible damage. This article explores the intricate relationship between diabetic retinopathy and severe insulin resistance, including pathophysiology, risk factors, and advanced treatment approaches.
Understanding Diabetic Retinopathy
Pathophysiology
Diabetic retinopathy is a progressive microvascular disorder caused by prolonged hyperglycemia, leading to retinal damage. The primary mechanisms involved include:
- Hyperglycemia-Induced Endothelial Dysfunction: Chronic high blood sugar damages the endothelial cells of retinal capillaries, increasing permeability and vessel fragility.
- Oxidative Stress and Inflammation: Elevated glucose levels generate reactive oxygen species (ROS), which trigger inflammation and further vascular damage.
- Neovascularization and Retinal Edema: In response to ischemia, the retina releases vascular endothelial growth factor (VEGF), leading to abnormal blood vessel formation and leakage.
Stages of Diabetic Retinopathy
- Non-Proliferative Diabetic Retinopathy (NPDR): Characterized by microaneurysms, retinal hemorrhages, and cotton wool spots.
- Proliferative Diabetic Retinopathy (PDR): Marked by neovascularization, which increases the risk of vitreous hemorrhage and retinal detachment.
- Diabetic Macular Edema (DME): Fluid accumulation in the macula, leading to central vision loss.
The Role of Severe Insulin Resistance in Diabetic Retinopathy
What is Severe Insulin Resistance?
Severe insulin resistance occurs when cells fail to respond effectively to insulin, requiring significantly higher doses to maintain glucose control. It is commonly associated with:
- Type 2 diabetes mellitus (T2DM)
- Obesity and metabolic syndrome
- Lipodystrophy and genetic insulin receptor mutations
How Severe Insulin Resistance Worsens Diabetic Retinopathy
- Increased Hyperglycemia: Poor insulin sensitivity results in persistent hyperglycemia, accelerating retinal damage.
- Dyslipidemia and Endothelial Dysfunction: Elevated triglycerides and free fatty acids contribute to vascular abnormalities.
- Chronic Inflammation: Systemic inflammation exacerbates oxidative stress, worsening microvascular complications.
- Resistance to Conventional Insulin Therapy: Patients with severe insulin resistance require high doses of insulin, which may cause fluctuations in blood glucose levels, further damaging the retina.
Mermaid Diagram: Pathophysiology of Diabetic Retinopathy in Severe Insulin Resistance
mermaidCopyEditgraph TD;
Hyperglycemia -->|Oxidative Stress| Endothelial_Dysfunction;
Hyperglycemia -->|Chronic Inflammation| Neovascularization;
Endothelial_Dysfunction -->|Retinal Ischemia| Neovascularization;
Neovascularization -->|Abnormal Vessel Growth| Retinal_Damage;
Retinal_Damage --> Vision_Loss;
Risk Factors for Diabetic Retinopathy in Severe Insulin Resistance
- Poor Glycemic Control: High HbA1c levels increase the risk of retinal complications.
- Hypertension: Elevated blood pressure exacerbates retinal vessel damage.
- Obesity and Dyslipidemia: Excess weight and abnormal lipid profiles accelerate microvascular injury.
- Genetic Predisposition: Family history of insulin resistance-related disorders may increase susceptibility.
- Duration of Diabetes: The longer the disease duration, the higher the risk of developing DR.
Advanced Management Strategies
Glycemic Optimization
- Metformin: First-line therapy for insulin resistance, improving glucose uptake.
- GLP-1 Receptor Agonists & SGLT2 Inhibitors: Reduce hyperglycemia and provide cardiovascular benefits.
- Insulin Sensitizers (Thiazolidinediones): Improve insulin sensitivity but require caution due to fluid retention risks.
Anti-VEGF Therapy for Retinal Protection
- Ranibizumab, Aflibercept, and Bevacizumab: Inhibit VEGF, reducing neovascularization and macular edema.
- Intravitreal Corticosteroids: Reduce inflammation but carry the risk of increased intraocular pressure.
Blood Pressure and Lipid Control
- ACE Inhibitors and ARBs: Protect retinal vessels by reducing hypertension.
- Statins and Fibrates: Lower LDL cholesterol and triglycerides, mitigating endothelial damage.
Lifestyle Modifications
- Diet: Low-glycemic, anti-inflammatory foods to stabilize blood sugar levels.
- Exercise: Regular physical activity enhances insulin sensitivity and cardiovascular health.
- Weight Management: Reducing body fat lowers insulin resistance and systemic inflammation.
Surgical Interventions for Advanced Cases
- Laser Photocoagulation: Seals leaking vessels, preventing further retinal damage.
- Vitrectomy: Removes vitreous hemorrhage and scar tissue in proliferative disease.