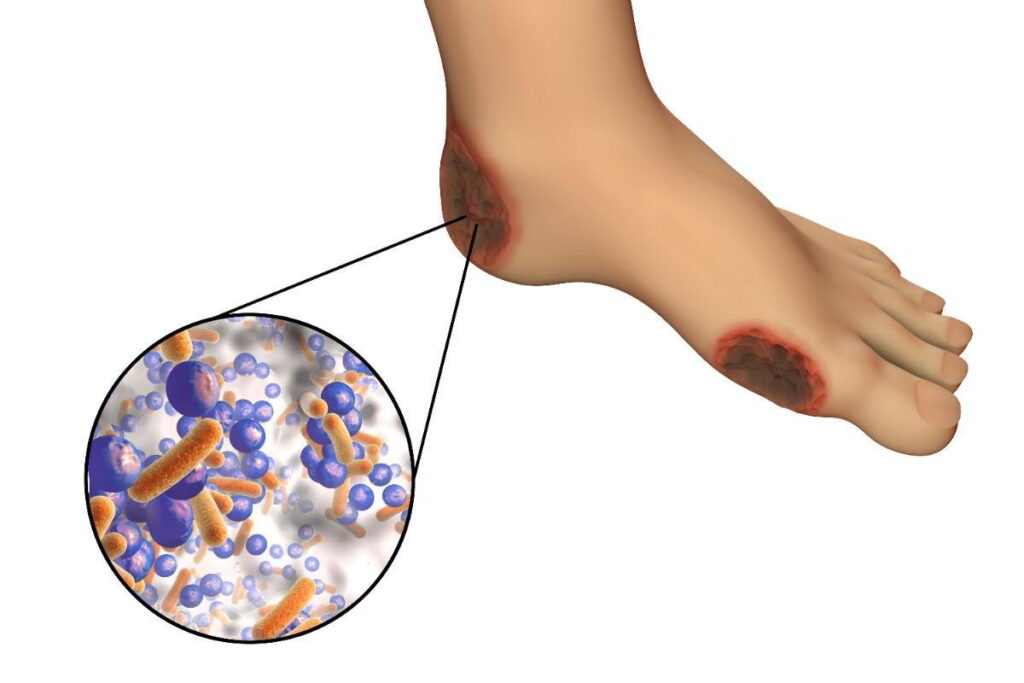
diabetic foot infection due to gram-positive bacteria are a significant complication in individuals with diabetes mellitus, particularly among those exhibiting severe insulin resistance. These infections often lead to substantial morbidity and can result in lower extremity amputations if not promptly and effectively managed. Gram-positive bacteria, notably Staphylococcus aureus and Streptococcus agalactiae, are frequently implicated in these infections. Understanding the interplay between severe insulin resistance and the susceptibility to gram-positive bacterial infections is crucial for developing effective prevention and treatment strategies.
Pathophysiology of Diabetic Foot Infections
The development of DFIs is multifactorial, involving a combination of neuropathy, peripheral arterial disease, and immune system impairments commonly associated with diabetes. Peripheral neuropathy leads to a loss of protective sensation, increasing the risk of unnoticed injuries. Peripheral arterial disease contributes to poor wound healing due to inadequate blood supply. Additionally, hyperglycemia adversely affects immune function, diminishing the body’s ability to combat infections. In the context of severe insulin resistance, these factors are often exacerbated, further elevating the risk of infection.
Microbiology: Gram-Positive Bacterial Pathogens
Gram-positive bacteria are predominant in DFIs, with Staphylococcus aureus being the most commonly isolated pathogen. Streptococcus agalactiae (Group B Streptococcus) is also frequently identified. These organisms can initiate infection through minor skin breaches, leading to cellulitis, abscess formation, and, in severe cases, osteomyelitis. The presence of methicillin-resistant Staphylococcus aureus (MRSA) has been increasingly reported, complicating treatment regimens.
Clinical Evaluation and Diagnosis
Early recognition of DFIs is vital to prevent progression to more severe disease states. Clinical signs indicative of infection include erythema, warmth, swelling, tenderness, and purulent discharge. In patients with severe insulin resistance, these signs may be subtle, necessitating a high index of suspicion. Diagnostic measures should encompass:
- Probe-to-Bone Test: Assessing for underlying osteomyelitis by probing the wound to detect bone involvement.
- Imaging Studies: Initial plain radiography to identify bone abnormalities, followed by magnetic resonance imaging (MRI) if osteomyelitis is suspected or if radiographs are inconclusive.
- Microbiological Assessment: Obtaining deep tissue or bone specimens for culture to identify causative organisms and determine antibiotic susceptibilities.
Management Strategies
Effective management of DFIs in patients with severe insulin resistance requires a multidisciplinary approach, including:
- Glycemic Control: Achieving optimal blood glucose levels to enhance immune function and promote wound healing.
- Antibiotic Therapy: Empirical antibiotic treatment should target gram-positive organisms, particularly Staphylococcus aureus and Streptococcus agalactiae. The choice of antibiotic should be guided by local resistance patterns and adjusted based on culture results. In cases of MRSA, agents such as linezolid or vancomycin may be considered. en.wikipedia.org
- Surgical Intervention: Prompt surgical debridement to remove necrotic tissue and drain abscesses is essential. In cases of osteomyelitis, more extensive surgical procedures may be necessary.
- Wound Care: Implementing appropriate wound care techniques, including regular dressing changes, offloading pressure from the affected area, and utilizing advanced wound care modalities as indicated.
Prevention Strategies
Preventing DFIs in individuals with severe insulin resistance involves:
- Patient Education: Educating patients on proper foot care, including daily inspection, hygiene practices, and the importance of prompt reporting of any foot abnormalities.
- Regular Screening: Conducting routine foot examinations to identify and address potential issues early.
- Footwear Assessment: Ensuring appropriate footwear to prevent pressure points and injuries.
- Management of Comorbidities: Addressing other contributing factors such as peripheral arterial disease and optimizing overall metabolic control.

