Acute Sinusitis Due to Klebsiella pneumoniae is a serious bacterial infection affecting the paranasal sinuses. As an opportunistic pathogen, K. pneumoniae primarily targets immunocompromised individuals, leading to severe sinus inflammation, mucus buildup, and potential complications. Early diagnosis and targeted treatment are crucial in managing the infection effectively.
Pathophysiology of Klebsiella pneumoniae-Induced Sinusitis
Klebsiella pneumoniae disrupts normal sinus flora, triggering inflammation and excessive mucus production, which can lead to obstruction of the sinus cavities. The bacterium’s thick polysaccharide capsule enhances virulence, enabling it to evade host immune responses and resist antibiotic treatment.
Risk Factors
Individuals at higher risk for K. pneumoniae-induced sinusitis include:
- Immunocompromised Patients: Those with diabetes, cancer, or HIV.
- Chronic Sinusitis Sufferers: Pre-existing inflammation creates a favorable environment.
- Hospitalized or Ventilator-Dependent Patients: Higher exposure to antibiotic-resistant strains.
- Smokers and Individuals with Respiratory Conditions: Impaired mucociliary clearance.
Clinical Symptoms
Patients with K. pneumoniae-induced acute sinusitis typically exhibit:
- Severe Facial Pain and Pressure: Concentrated around the affected sinuses.
- Purulent Nasal Discharge: Thick, yellow-green mucus.
- Nasal Congestion and Postnasal Drip: Worsening breathing difficulty.
- Fever and Fatigue: Indicative of systemic infection.
- Headache and Sinus Tenderness: Especially around the forehead and cheeks.
Diagnosis
A thorough evaluation is necessary to confirm Klebsiella pneumoniae as the causative pathogen:
- Clinical Examination: Assessment of symptoms and medical history.
- Nasal Endoscopy: Direct visualization of sinus inflammation and mucus buildup.
- Microbiological Testing: Sinus aspirate cultures to identify K. pneumoniae.
- Imaging Studies: CT scans reveal sinus blockage and potential complications.
- Blood Tests: Elevated white blood cell count and inflammatory markers.
Treatment Strategies
1. Antibiotic Therapy
- First-line antibiotics: Third-generation cephalosporins (ceftriaxone, cefotaxime).
- Carbapenems: Recommended for multidrug-resistant K. pneumoniae strains.
- Aminoglycosides and Fluoroquinolones: Used in severe cases or hospital-acquired infections.
2. Symptom Management
- Nasal Decongestants: Oxymetazoline or pseudoephedrine to reduce nasal swelling.
- Saline Irrigation: Clears mucus buildup and improves sinus drainage.
- Pain Relievers: NSAIDs such as ibuprofen alleviate headache and facial pain.
3. Surgical Intervention
- Functional Endoscopic Sinus Surgery (FESS): Removes obstructions and restores normal drainage in refractory cases.
- Sinus Drainage Procedures: Required for abscesses or chronic infections.
Prevention Strategies
- Good Hygiene Practices: Frequent handwashing minimizes bacterial exposure.
- Avoiding Smoking and Pollutants: Preserves sinus mucosal integrity.
- Proper Use of Medical Devices: Reduces risk in ventilated or hospitalized patients.
- Early Treatment of Upper Respiratory Infections: Prevents bacterial superinfection.
Prognosis and Complications
If untreated, K. pneumoniae-induced sinusitis may lead to:
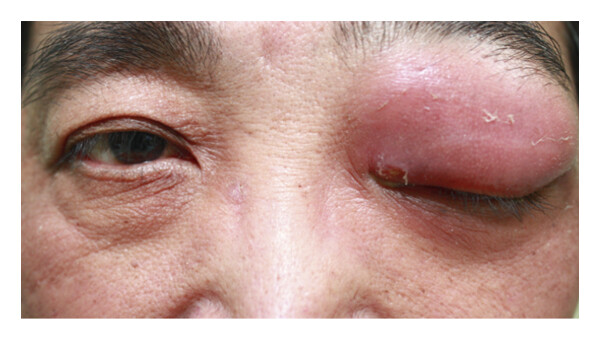
- Orbital Cellulitis: Infection spreading to the eye socket.
- Meningitis: Bacterial invasion of the central nervous system.
- Septicemia: Systemic spread resulting in life-threatening complications.
- Chronic Sinus Damage: Persistent inflammation leading to structural changes.
Prompt medical intervention significantly reduces the risk of complications and improves patient outcomes.
Acute sinusitis due to Klebsiella pneumoniae is a serious condition that demands early diagnosis and appropriate antibiotic therapy. Comprehensive management includes antimicrobial treatment, symptom relief, and, in severe cases, surgical intervention. Preventative measures are essential to reduce the risk of recurrence and complications.