Depressive type psychosisdermatitis herpetiformis is a chronic, autoimmune skin condition characterized by intensely itchy, blistering rashes. It is closely associated with celiac disease, an immune response to gluten ingestion. Recent studies have highlighted a potential connection between DH and various psychiatric manifestations, particularly depressive disorders. This article aims to provide a comprehensive overview of DH, its association with depressive disorders, and the implications for patient care.

Depressive type psychosisdermatitis herpetiformis: An Overview
Pathophysiology and Clinical Presentation
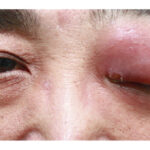
DH is considered the skin manifestation of celiac disease. When individuals with DH consume gluten—a protein found in wheat, barley, and rye—their immune system produces Immunoglobulin A (IgA) antibodies. These antibodies target epidermal transglutaminase, leading to the deposition of IgA in the dermal papillae. This immune response results in the characteristic symptoms of DH, which include:
- Intensely itchy, blistering skin lesions: These typically appear symmetrically on extensor surfaces such as the elbows, knees, buttocks, and scalp.
- Chronic and relapsing course: Symptoms may fluctuate, often exacerbated by gluten ingestion.
Diagnosis is confirmed through a skin biopsy, revealing granular IgA deposits in the dermal papillae. Serological tests for celiac disease-related antibodies may also support the diagnosis.
Management Strategies
The cornerstone of DH management is a strict, lifelong gluten-free diet (GFD), which addresses both the skin manifestations and the underlying intestinal sensitivity. Adherence to a GFD can lead to the resolution of skin lesions and prevent potential complications associated with celiac disease. In cases where immediate symptom relief is necessary, medications such as dapsone may be prescribed due to their anti-inflammatory properties. However, dapsone does not address the underlying cause, and its use requires monitoring for potential side effects.
The Association Between DH and Depressive Disorders
Exploring the Connection
Emerging evidence suggests a link between DH and various psychiatric conditions, notably depressive disorders. Several mechanisms have been proposed to explain this association:
- Nutritional Deficiencies: Malabsorption in celiac disease can lead to deficiencies in essential nutrients like B vitamins and iron, which are crucial for neurological function and mood regulation.
- Immune System Dysregulation: Chronic inflammation and immune responses may influence brain function, potentially contributing to mood disorders.
- Psychosocial Impact: The chronic, visible nature of DH can affect self-esteem and social interactions, potentially leading to depressive symptoms.
A case report highlighted a patient with DH who experienced exacerbation of depressive symptoms during flare-ups of the skin condition, suggesting a temporal relationship between skin inflammation and mood changes.
Implications for Patient Care
Recognizing the potential link between DH and depressive disorders is vital for comprehensive patient care. Healthcare providers should:
- Screen for Psychiatric Symptoms: Regular assessments for depression and anxiety in patients with DH can facilitate early identification and intervention.
- Collaborate with Mental Health Professionals: Integrated care approaches can address both dermatological and psychological aspects, improving overall patient outcomes.
- Educate Patients: Informing patients about the possible connection between DH and mood disorders can encourage them to report symptoms promptly.