Denture stomatitis, also known as denture-induced stomatitis or chronic atrophic candidiasis, is a prevalent inflammatory condition affecting individuals who wear removable dentures. It is characterized by erythema and swelling of the oral mucosa in areas covered by the denture. This condition is commonly associated with the overgrowth of Candida species, particularly Candida albicans, and is influenced by various local and systemic factors.
Etiology and Risk Factors
The development of denture stomatitis is multifactorial, involving both local and systemic contributors:
Local Factors
Systemic Factors
- Age: Elderly individuals are more susceptible due to age-related changes in oral mucosa and immune function.
- Medications: Prolonged use of broad-spectrum antibiotics and corticosteroids can disrupt the normal oral flora, promoting fungal overgrowth.
Clinical Presentation
Denture stomatitis typically presents as:
- Erythema: Redness of the mucosa beneath the denture.
- Edema: Swelling in the affected areas.
- Petechial Hemorrhages: Small red spots due to minor bleeding.
Patients may be asymptomatic or report discomfort, burning sensations, or unpleasant taste. The condition is often classified into three types:
- Type I: Localized inflammation or pinpoint hyperemia.
- Type II: Diffuse erythema involving a broader area of the mucosa.
- Type III: Granular or papillary hyperplasia, commonly seen on the hard palate.
Diagnosis
Diagnosis is primarily clinical, based on the characteristic appearance of the mucosa under the denture. To confirm the presence of Candida species, a swab of the affected area can be taken for microbiological analysis. In certain cases, a biopsy may be performed to rule out other mucosal pathologies.
Management and Treatment
Effective management of denture stomatitis involves a combination of mechanical, chemical, and behavioral strategies:
Mechanical Measures
- Denture Removal: Patients should be advised to remove dentures during sleep to reduce mucosal exposure time and allow tissue recovery.
Chemical Measures
- Antifungal Therapy: Topical antifungal agents, such as nystatin or miconazole gels, can be applied to the affected mucosa and the fitting surface of the denture. In refractory cases, systemic antifungal medications may be prescribed.
- Denture Disinfection: Soaking dentures in antifungal solutions can help eradicate fungal biofilms. However, care must be taken to avoid solutions that may damage denture materials.
Behavioral and Preventive Measures
- Dietary Modifications: Reducing sugar intake can help limit fungal growth.
- Smoking Cessation: Encouraging patients to quit smoking can improve treatment outcomes, as smoking is a known risk factor for denture stomatitis.
- Regular Dental Check-Ups: Routine visits to a dental professional for denture assessment and oral examination are crucial for early detection and management.
Prevention
Preventive strategies are paramount in reducing the incidence of denture stomatitis:
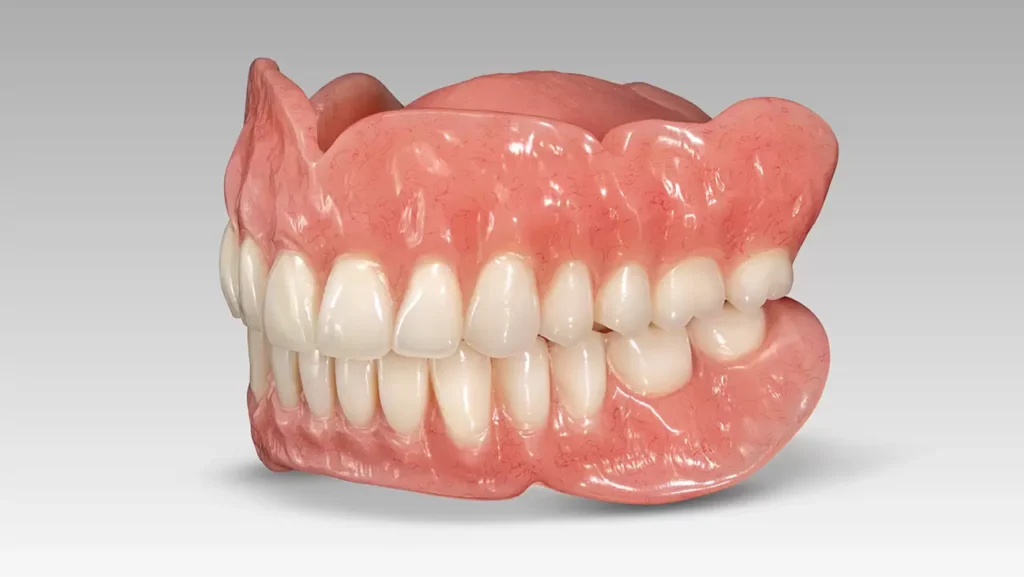
- Proper Denture Fabrication: Ensuring dentures are well-fitted to minimize trauma and areas where plaque can accumulate.
- Patient Education: Informing patients about the importance of denture hygiene, regular removal, and the risks associated with continuous wear.
- Monitoring Systemic Health: Managing underlying systemic conditions, such as diabetes, can reduce susceptibility to infections.