Cytomegalovirus diseaseis a member of the Herpesviridae family and is a prevalent virus affecting individuals of all ages. While many infections remain asymptomatic, CMV poses a serious threat to immunocompromised individuals and newborns with congenital infection. Understanding its transmission, clinical manifestations, diagnosis, and management is essential for effective disease prevention and control.
Transmission and Epidemiology
CMV spreads through direct contact with bodily fluids, including saliva, urine, blood, tears, semen, and breast milk. Key transmission routes include:
- Person-to-person contact: Through saliva, sexual contact, or close household exposure.
- Congenital transmission: From mother to fetus during pregnancy.
- Blood transfusion and organ transplantation: Transmission can occur in immunocompromised recipients.
- Breastfeeding: CMV can be transmitted from mother to infant through breast milk.
The virus is widespread, with most adults being infected by middle age. Infection rates vary by region, with higher prevalence in developing countries.
Clinical Manifestations
Asymptomatic and Mild Infections
Most healthy individuals with CMV experience no symptoms or mild flu-like illness, including:
- Fever
- Fatigue
- Swollen lymph nodes
- Muscle aches
CMV in Immunocompromised Patients
In individuals with weakened immune systems, such as transplant recipients, cancer patients, and those with HIV/AIDS, CMV can cause severe complications, including:
- CMV Retinitis: Can lead to vision loss.
- CMV Pneumonitis: Lung infection causing respiratory distress.
- CMV Hepatitis: Liver inflammation.
- CMV Colitis: Gastrointestinal infection leading to diarrhea and ulcers.
- CMV Encephalitis: Brain inflammation causing neurological impairment.
Congenital CMV Infection
Congenital CMV occurs when an infected mother passes the virus to her fetus. It is a leading cause of birth defects and long-term disabilities. Symptoms may include:
- Low birth weight
- Jaundice
- Microcephaly (small head size)
- Seizures
- Hearing and vision loss
- Developmental delays
Diagnosis
CMV infection is diagnosed through laboratory tests, including:
- Serology: Detects CMV-specific IgM and IgG antibodies to indicate recent or past infection.
- Polymerase Chain Reaction (PCR): Identifies CMV DNA in blood, urine, or saliva.
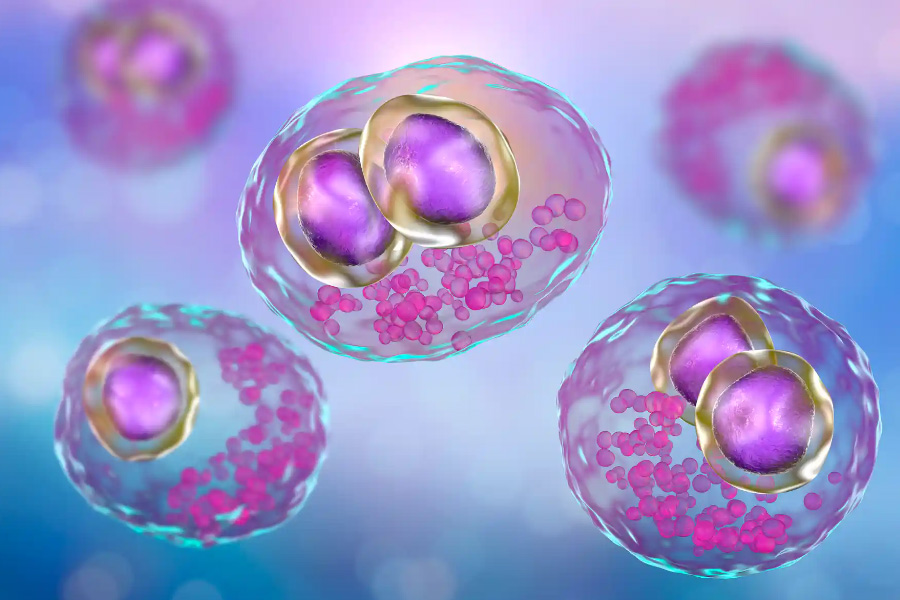
- Histopathology: Identifies characteristic “owl’s eye” intranuclear inclusions in tissue samples.
- Viral Culture: Confirms CMV presence in clinical specimens.
For congenital CMV, testing must be conducted within the first three weeks of life to confirm infection.
Management and Treatment
Immunocompetent Individuals
Most healthy individuals do not require treatment, as CMV infections are self-limiting.
Immunocompromised Patients
Antiviral medications are used to manage severe CMV infections:
- Ganciclovir: First-line intravenous treatment for severe cases.
- Valganciclovir: Oral prodrug of ganciclovir used for long-term therapy.
- Foscarnet and Cidofovir: Alternatives for resistant cases or patients who cannot tolerate ganciclovir.
Congenital CMV
Newborns with symptomatic congenital CMV may benefit from antiviral therapy to reduce long-term complications. However, treatment decisions depend on the severity of symptoms and potential drug-related side effects.
Prevention
Since no CMV vaccine is currently available, preventive strategies focus on hygiene and infection control:
- Frequent handwashing: Reduces the risk of transmission.
- Avoid sharing personal items: Such as utensils and drinks with young children.
- Safe sex practices: Using protection can reduce sexual transmission.
- Screening of blood and organ donors: Minimizes CMV transmission in transplant recipients.
- Pregnancy precautions: Pregnant individuals should practice extra caution around young children and their bodily fluids.