Cryptorchidism, commonly known as an undescended testicle, is a condition in which one or both testicles fail to move into the scrotum before birth. This condition affects approximately 3% of full-term and 30% of preterm male infants. Left untreated, cryptorchidism can lead to fertility issues and an increased risk of testicular cancer.
What is Cryptorchidism?
Cryptorchidism refers to the failure of one or both testicles to descend into the scrotum. Normally, the testes develop in the abdomen and descend into the scrotal sac during fetal development. When this process is incomplete, the testicle remains in the abdomen or groin.
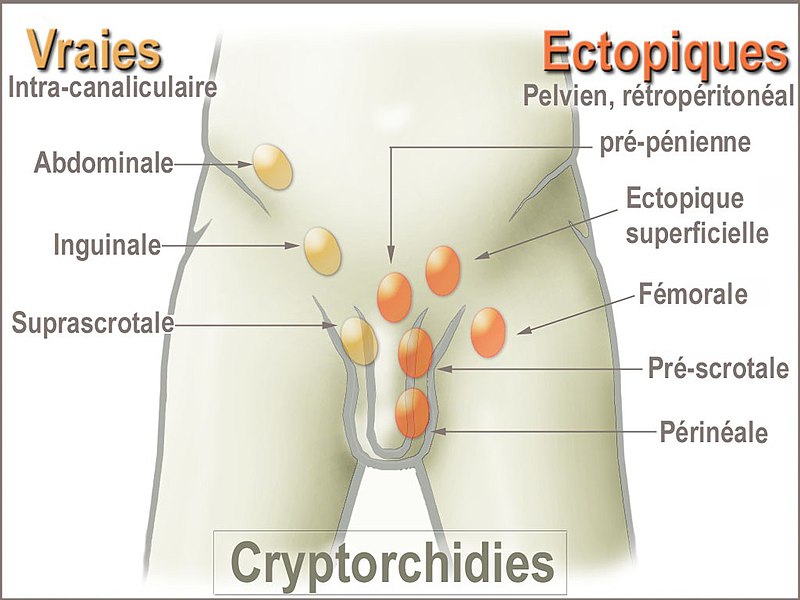
Types of Cryptorchidism
- Unilateral Cryptorchidism: One testicle remains undescended.
- Bilateral Cryptorchidism: Both testicles fail to descend.
- Retractile Testicle: A testicle that moves in and out of the scrotum due to an overactive cremaster muscle.
- Ectopic Testicle: A testicle that moves to an abnormal location outside the normal descent path.
Causes and Risk Factors
Causes
- Hormonal imbalances during fetal development
- Genetic mutations affecting testicular descent
- Mechanical obstructions preventing testicular movement
Risk Factors
- Premature birth
- Low birth weight
- Family history of cryptorchidism
- Maternal smoking or alcohol use during pregnancy
- Exposure to endocrine-disrupting chemicals
Symptoms and Complications
Symptoms
- Absence of one or both testicles in the scrotum
- Asymmetrical scrotum
- Palpable testicle in the groin
Complications
- Infertility: Increased temperature in the abdomen or groin may impair sperm production.
- Testicular Cancer: Higher risk due to abnormal testicular development.
- Hernia Development: Associated with an inguinal hernia.
- Testicular Torsion: Twisting of the testicle, leading to reduced blood supply.
Diagnosis
Physical Examination
A pediatrician or urologist performs a thorough examination to locate the undescended testicle.
Imaging Tests
- Ultrasound: Helps detect the location of the testicle.
- MRI: Provides detailed imaging for non-palpable testes.
Hormonal Tests
- hCG Stimulation Test: Evaluates testosterone production to confirm the presence of testicular tissue.
Treatment Options
Observation and Spontaneous Descent
In many cases, testicular descent occurs naturally within six months of birth. If the testicle has not descended by this time, medical intervention is required.
Hormone Therapy
- hCG (Human Chorionic Gonadotropin): Stimulates testicular descent.
- GnRH (Gonadotropin-Releasing Hormone): Used in select cases to induce descent.
Surgical Treatment
The standard treatment for cryptorchidism is orchiopexy, a surgical procedure to move the testicle into the scrotum.
Long-Term Outlook and Follow-Up Care
Regular follow-ups are essential to monitor testicular function and detect potential complications.
Monitoring Fertility
- Semen analysis in adulthood
- Hormone level assessments
Testicular Cancer Screening
Men with a history of cryptorchidism should perform regular testicular self-exams and undergo periodic medical evaluations.

