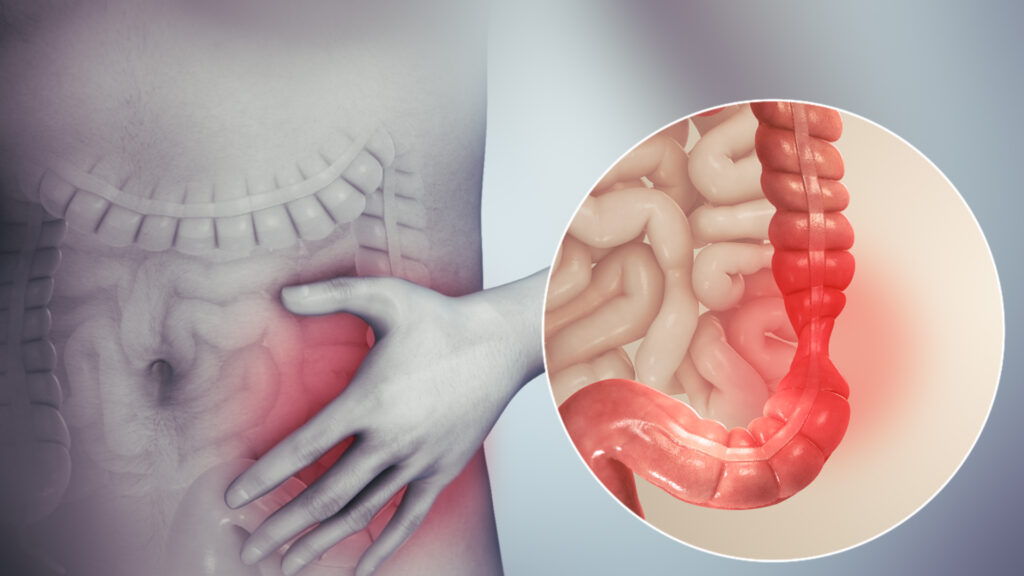
Constipation predominant irritable bowel syndrome (IBS-C) is a gastrointestinal disorder affecting millions worldwide. Characterized by chronic constipation, bloating, and discomfort, it often disrupts daily life and overall well-being. In this comprehensive guide, we delve into IBS-C’s causes, symptoms, diagnostic process, and available treatment options. Our goal is to provide the most up-to-date and accurate information to help individuals manage and overcome this challenging condition.
What is Constipation Predominant Irritable Bowel Syndrome?
Constipation predominant irritable bowel syndrome (IBS-C) is a subtype of IBS where individuals experience infrequent, difficult-to-pass stools alongside other symptoms like bloating, abdominal pain, and discomfort. Unlike typical constipation, which may occur due to diet, dehydration, or medication, IBS-C is a chronic condition that requires long-term management and attention to avoid complications.
The primary symptoms of IBS-C include:
- Infrequent bowel movements: Less than three bowel movements per week.
- Hard or lumpy stools: Stool consistency may be tough, leading to straining during bowel movements.
- Abdominal discomfort and bloating: Common feelings of fullness and pain that are relieved after bowel movements.
IBS-C vs. Other Types of IBS
IBS is generally classified into four subtypes based on predominant symptoms:
- IBS with constipation (IBS-C)
- IBS with diarrhea (IBS-D)
- IBS with mixed bowel habits (IBS-M)
- Unclassified IBS (IBS-U)
IBS-C is unique in its focus on constipation, while other subtypes may include symptoms like diarrhea or alternating between the two. Understanding the specific type of IBS is crucial for tailoring effective treatment options.
Causes and Risk Factors of IBS-C
The exact cause of IBS-C remains unclear, but several factors may contribute to the development of this condition. These include:
1. Gastrointestinal Motility Issues
The most common contributing factor to IBS-C is altered motility within the gut. Slow-moving digestive muscles lead to constipation as the movement of stool through the intestines becomes sluggish. This results in hard, dry stools that are difficult to pass.
2. Gut Microbiome Imbalance
Research suggests that an imbalance in gut bacteria may play a role in IBS-C. The presence of harmful bacteria or a lack of beneficial bacteria may disrupt normal digestion and contribute to the symptoms of constipation.
3. Visceral Hypersensitivity
Individuals with IBS-C often experience increased sensitivity to stimuli within the intestines. This heightened pain perception may lead to abdominal discomfort, bloating, and changes in bowel function.
4. Psychological Factors
Stress, anxiety, and depression have long been linked to IBS. Psychological distress can worsen gut motility and amplify gastrointestinal symptoms. A history of trauma or emotional factors may also be a contributing cause.
5. Genetic Predisposition
There may be a hereditary component to IBS-C. Family members of individuals with IBS-C are more likely to experience the condition themselves, suggesting a genetic or familial influence.
6. Infections and Antibiotics
Some cases of IBS-C may develop after an infection or a course of antibiotics. This phenomenon, known as post-infectious IBS, may cause a disturbance in the gut’s normal function, leading to symptoms such as constipation.
Recognizing the Symptoms of IBS-C
The symptoms of constipation predominant IBS can be disruptive and distressing. Individuals with IBS-C commonly report the following signs:
1. Chronic Constipation
This is the hallmark symptom of IBS-C. Bowel movements may occur less than three times per week, often with difficulty and straining.
2. Abdominal Discomfort and Pain
Frequent bloating, cramps, and a sensation of fullness are common complaints. These symptoms are often relieved by passing stool but may return shortly after.
3. Hard, Lumpy Stools
Stools in IBS-C are typically dry and hard, making them difficult to pass. In some cases, individuals may feel that they have not completely emptied their bowels after a movement.
4. Bloating and Gas
Excessive gas buildup is often reported, contributing to bloating and distention of the abdomen. This discomfort can occur at any time but is typically more intense after meals.
5. Mucus in Stool
Some individuals with IBS-C may notice the presence of mucus in their stool. While this is not uncommon in IBS, it is especially associated with bloating and constipation.
Diagnosing IBS-C
Diagnosis of IBS-C involves a thorough evaluation of symptoms, medical history, and lifestyle factors. There is no single test for IBS, but doctors may use a combination of the following methods to confirm the condition:
1. Rome IV Criteria
The Rome IV criteria are widely used to diagnose IBS. To meet the criteria for IBS-C, a patient must have experienced abdominal discomfort or pain for at least one day per week over the last three months, with symptoms starting at least six months ago. Additionally, individuals must meet two or more of the following conditions:
- Pain or discomfort relieved by bowel movements
- A change in frequency of stool
- A change in stool form or consistency
2. Exclusion of Other Conditions
To ensure the symptoms are not caused by another condition, doctors may recommend tests such as blood work, stool analysis, and imaging studies. Conditions like celiac disease, colon cancer, and thyroid dysfunction must be ruled out.
3. Colonoscopy or Endoscopy
In some cases, a colonoscopy or endoscopy may be used to examine the intestines and identify any abnormalities. This is generally recommended if there are alarm symptoms such as unexplained weight loss, blood in stool, or a family history of colon cancer.
Effective Treatment Options for IBS-C
Managing constipation predominant irritable bowel syndrome requires a multifaceted approach. While there is no cure, a combination of dietary modifications, medications, and lifestyle changes can help alleviate symptoms and improve quality of life.
1. Dietary Modifications
Diet plays a crucial role in managing IBS-C. The following dietary changes can help:
- Increase fiber intake: Soluble fiber, found in foods like oats, fruits, and vegetables, can help soften stools and improve bowel movements.
- Limit FODMAPs: The low-FODMAP diet restricts certain fermentable carbohydrates that can cause bloating and gas. Working with a dietitian can help personalize this approach.
- Stay hydrated: Drinking plenty of fluids helps prevent stool hardening and promotes smoother digestion.
2. Medications
Several medications may be prescribed to treat IBS-C:
- Laxatives: For short-term relief, laxatives like polyethylene glycol can help soften stools and relieve constipation.
- Prokinetics: These medications improve gut motility by stimulating intestinal muscles, making bowel movements easier.
- Antispasmodics: Used to reduce abdominal cramping and discomfort, antispasmodics like hyoscyamine can provide symptom relief.
- Antidepressants: Low-dose antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs), may help reduce pain perception and regulate bowel function.
3. Psychological Support
Since stress and psychological factors can exacerbate IBS-C symptoms, cognitive behavioral therapy (CBT) and mindfulness techniques may be beneficial. Additionally, regular physical activity can help reduce stress and improve gut motility.
4. Probiotics
The use of probiotics, which introduce beneficial bacteria into the gut, may help restore a balanced microbiome. This could reduce bloating and other IBS-C symptoms in some individuals.
Long-Term Management and Lifestyle Tips
Managing IBS-C is an ongoing process, and individuals may need to experiment with different treatment strategies to find what works best for them. Regular follow-up with healthcare providers is essential to adjust treatment plans as necessary.
Some additional lifestyle tips to manage IBS-C include:
- Regular exercise: Physical activity helps stimulate bowel movement and reduce stress.
- Mindful eating: Eating slowly and chewing food thoroughly can reduce bloating and discomfort.
- Sleep hygiene: Maintaining a regular sleep schedule supports overall digestive health and reduces stress levels.