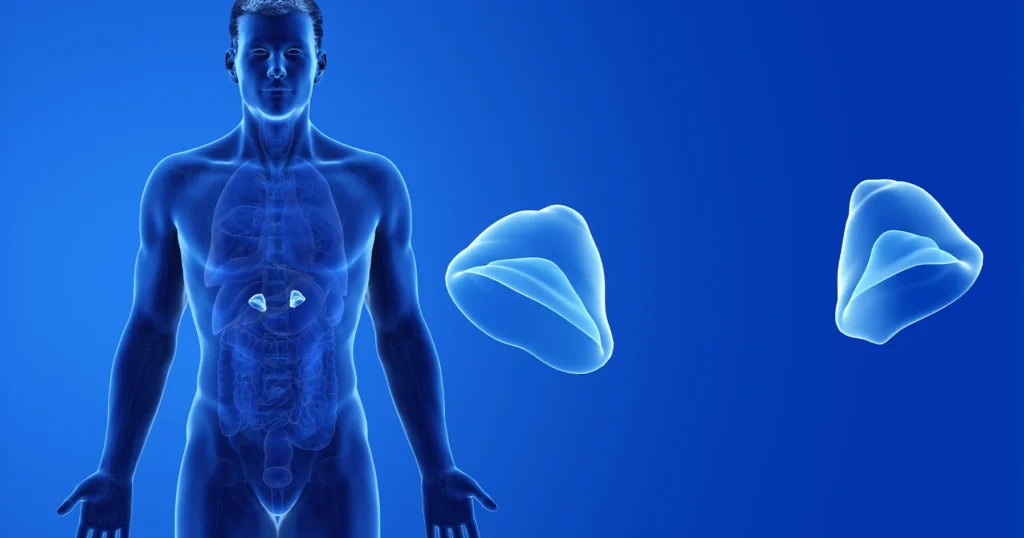
Congenital Adrenal Hyperplasia (CAH) encompasses a group of inherited disorders affecting the adrenal glands, leading to hormone imbalances that can significantly impact health. This article delves into the causes, symptoms, diagnostic procedures, and treatment options for CAH, providing a thorough understanding of this condition.
Understanding Congenital Adrenal Hyperplasia
CAH is primarily characterized by a deficiency in one of the enzymes necessary for cortisol production in the adrenal glands. The most prevalent form, accounting for approximately 95% of cases, is due to 21-hydroxylase deficiency. This enzyme deficiency disrupts the synthesis of cortisol and often aldosterone, leading to an overproduction of androgens, which are male sex hormones.
Types of CAH
CAH is categorized mainly into two forms:
- Classic CAH: This severe form is evident at birth and is further divided into:
- Salt-Losing CAH: Characterized by a significant loss of sodium, leading to life-threatening dehydration if untreated.
- Simple-Virilizing CAH: Does not involve salt loss but leads to the development of male physical characteristics (virilization) due to excess androgen production.
- Non-Classic CAH: A milder form that may not become apparent until later in life, often during adolescence or adulthood. Symptoms can include mild virilization and fertility issues.
Causes and Genetic Basis
CAH is an autosomal recessive disorder, meaning an individual must inherit two copies of the defective gene, one from each parent, to manifest the condition. The most common cause is mutations in the CYP21A2 gene, which encodes the 21-hydroxylase enzyme. This mutation impairs the adrenal glands’ ability to produce cortisol and aldosterone effectively.
Clinical Manifestations
The symptoms of CAH vary depending on the type and severity of the enzyme deficiency:
- Classic CAH:
- Females: May present with ambiguous genitalia at birth due to excess androgen exposure.
- Males: Typically have normal genitalia but may exhibit signs of early puberty.
- Both Genders: Risk of adrenal crisis characterized by vomiting, dehydration, low blood pressure, and hypoglycemia.
- Non-Classic CAH:
- Females: Irregular menstrual cycles, hirsutism (excessive hair growth), and acne.
- Males: Early onset of puberty and rapid growth during childhood but shorter final adult height.
- Both Genders: Potential fertility challenges.
Diagnostic Approaches
Diagnosis of CAH involves a combination of clinical evaluation and laboratory testing:
- Newborn Screening: Routine in many countries, measuring 17-hydroxyprogesterone levels to detect classic CAH early.
- Hormonal Assays: Blood tests to assess levels of cortisol, aldosterone, and androgens.
- Genetic Testing: Identifying mutations in the CYP21A2 gene to confirm the diagnosis and inform family planning.
Treatment Strategies
Management of CAH focuses on hormone replacement and symptom control:
- Glucocorticoids: Administered to replace deficient cortisol and suppress excess androgen production.
- Mineralocorticoids: Prescribed for individuals with salt-losing CAH to maintain sodium balance and blood pressure.
- Surgical Intervention: In females with significant virilization, reconstructive surgery may be considered to address ambiguous genitalia.
- Monitoring and Support: Regular follow-ups with an endocrinologist, psychological support, and patient education are crucial components of comprehensive care.
Recent Developments
Advancements in treatment options have emerged, such as the FDA’s approval of Neurocrine Biosciences’ drug, Crenessity, for treating classic CAH in individuals aged four years and older. This medication, used alongside glucocorticoids, helps reduce excessive androgen production, offering a new avenue for managing this condition.

