Acetaminophen overdose is a critical medical emergency that requires prompt recognition and treatment. This guide explores the causes, risk factors, clinical presentation, diagnostic approaches, and management strategies for acetaminophen toxicity. By understanding these aspects, healthcare providers and individuals can mitigate the risks associated with this potentially fatal condition.
Understanding Acetaminophen Overdose
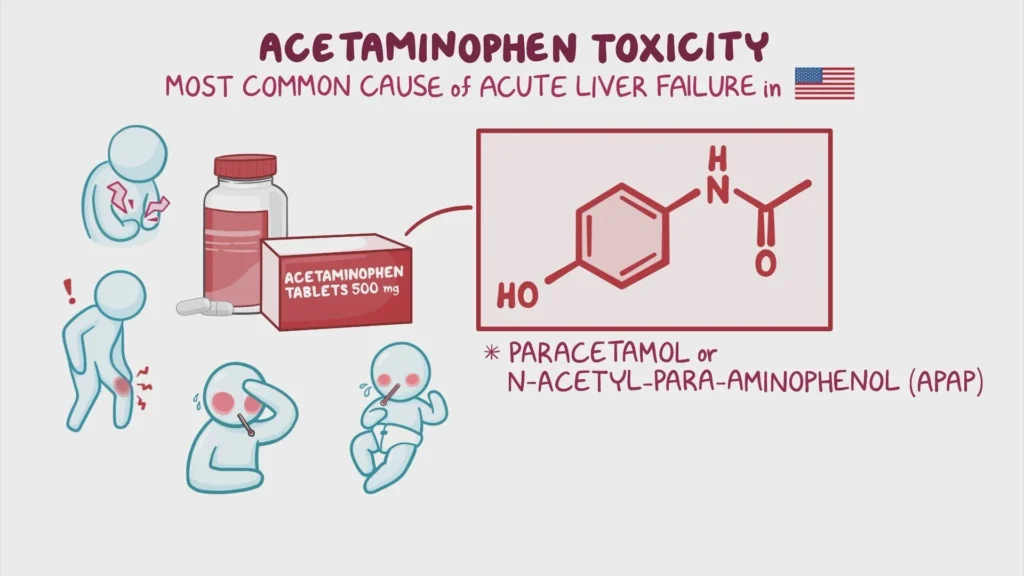
Acetaminophen, also known as paracetamol, is a commonly used over-the-counter medication for pain relief and fever reduction. While safe at recommended doses, excessive consumption can lead to severe liver damage and even death. Overdose can occur through a single large ingestion or repeated excessive doses over time.
Causes and Risk Factors for Acetaminophen Overdose
Common Causes
- Intentional Overdose: Often associated with self-harm or suicide attempts.
- Unintentional Overdose: Results from:
- Taking multiple medications containing acetaminophen.
- Miscalculating the correct dose, especially in children.
Risk Factors
- Chronic alcohol use (reduces liver’s ability to metabolize acetaminophen).
- Pre-existing liver diseases (e.g., hepatitis, cirrhosis).
- Use of enzyme-inducing drugs (e.g., phenytoin, carbamazepine).
Mechanism of Acetaminophen Toxicity
Acetaminophen is metabolized in the liver through conjugation pathways into non-toxic metabolites. However, a portion is converted to a highly reactive compound, N-acetyl-p-benzoquinone imine (NAPQI). At therapeutic doses, glutathione neutralizes NAPQI. In overdose situations, glutathione stores are depleted, allowing NAPQI to damage liver cells.
Symptoms and Clinical Presentation of Acetaminophen Overdose
The clinical progression of acetaminophen toxicity occurs in four distinct stages:
Stage 1 (0–24 Hours): Initial Symptoms
- Nausea
- Vomiting
- Abdominal pain
- General malaise
Stage 2 (24–72 Hours): Latent Phase
- Symptoms may subside, but liver damage progresses.
- Elevated liver enzymes (ALT, AST) and bilirubin levels.
Stage 3 (72–96 Hours): Maximum Liver Injury
- Jaundice
- Coagulopathy
- Hypoglycemia
- Acute renal failure in some cases
- Potential for multi-organ failure
Stage 4 (4–14 Days): Recovery or Death
- Recovery phase involves liver regeneration.
- Severe cases may progress to irreversible liver failure.
Diagnosis of Acetaminophen Overdose
Key Diagnostic Tools
- Patient History: Timing and amount of acetaminophen ingested.
- Serum Acetaminophen Levels: Measured using the Rumack-Matthew nomogram to assess the risk of liver toxicity.
- Liver Function Tests: Elevated ALT, AST, and bilirubin levels indicate liver injury.
- Coagulation Profile: Prolonged prothrombin time (PT) reflects impaired liver function.
Management and Treatment of Acetaminophen Overdose
Immediate Steps
- Activated Charcoal: Administered within 1–4 hours of ingestion to reduce absorption in the gastrointestinal tract.
Antidote: N-Acetylcysteine (NAC)
NAC replenishes glutathione levels and neutralizes NAPQI. It is most effective when administered within 8 hours of overdose.
NAC Administration Routes
- Oral NAC: Typically given in multiple doses.
- Intravenous NAC: Preferred for severe cases or if oral administration is not feasible.
Supportive Care
- Monitoring vital signs, liver function, and renal function.
- Managing complications such as hypoglycemia or coagulopathy.
- Liver Transplantation: Reserved for cases of fulminant hepatic failure.
Prevention of Acetaminophen Overdose
- Education: Raise awareness about the risks of overdose and proper dosing.
- Prescription Practices: Avoid prescribing multiple medications containing acetaminophen.
- Packaging: Use child-resistant packaging and limit package sizes.
- Monitoring at-Risk Patients: Regularly review medication use in patients with a history of substance abuse or mental health conditions.
Long-Term Outlook
Patients who receive timely treatment often recover fully from acetaminophen overdose. However, delayed treatment may result in permanent liver damage or death. Prevention and education remain critical in reducing the incidence of this preventable medical emergency.