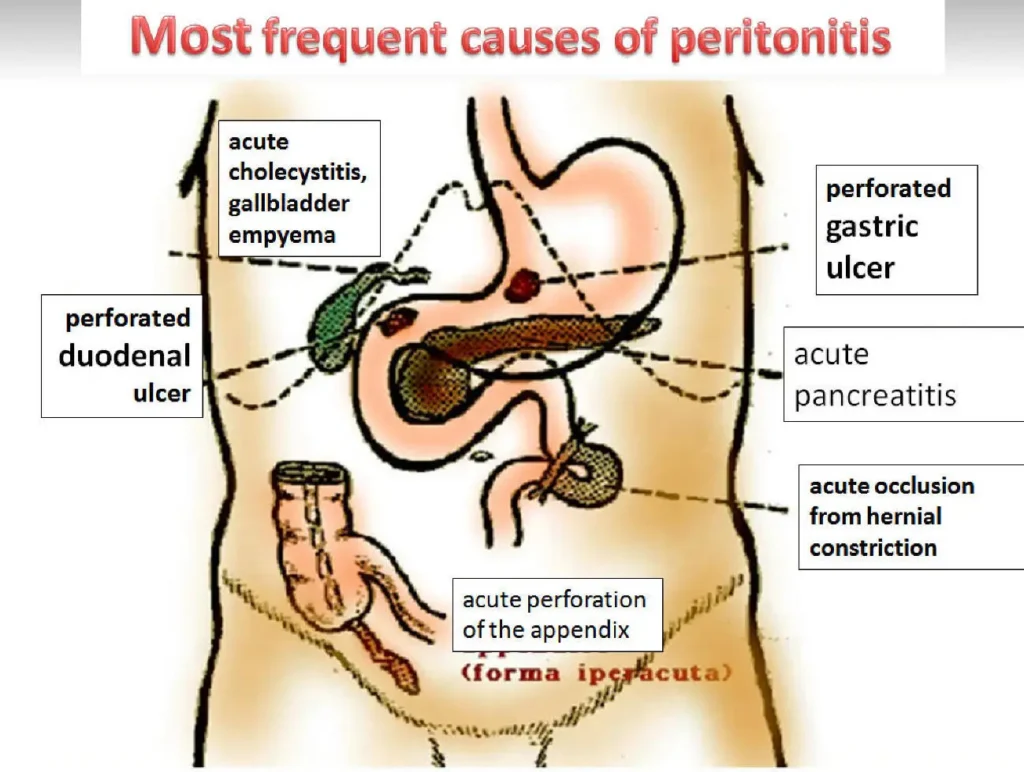
Peritonitis is an acute and often life-threatening condition characterized by the inflammation of the peritoneum, the membrane lining the abdominal cavity. When complicated peritonitis occurs due to infections by less common bacteria such as Eubacterium, the condition becomes even more challenging to diagnose and treat. This article delves into the complexities of complicated peritonitis caused by Eubacterium, providing in-depth insights into the infection’s pathophysiology, clinical manifestations, diagnostic methods, and treatment approaches.
What is Complicated Peritonitis?
Complicated peritonitis refers to peritoneal inflammation that results from a microbial infection, often with serious consequences such as organ failure or sepsis. The infection can arise from a range of pathogens, but Eubacterium, a genus of anaerobic bacteria, is a notable cause. These bacteria are typically part of the normal flora in the human gastrointestinal tract but can lead to severe infections under specific conditions.
Complicated peritonitis is characterized by:
- Widespread inflammation
- Bacterial growth that may spread throughout the abdominal cavity
- Potential for systemic infection and sepsis
This form of peritonitis can lead to abdominal distension, pain, fever, and shock, and it typically requires immediate medical intervention.
The Role of Eubacterium in Peritonitis
Eubacterium is an anaerobic bacterium that is naturally found in the intestines, where it helps digest food and maintain a healthy gut microbiome. However, under certain circumstances, such as after trauma, surgery, or bowel perforation, Eubacterium can migrate from the gastrointestinal tract to the peritoneal cavity, causing infection.
Infections caused by Eubacterium are often mixed, involving multiple pathogens, including other anaerobes and facultative organisms. This polymicrobial nature complicates diagnosis and treatment, as physicians must address the unique characteristics of both aerobic and anaerobic bacteria.
Common Species of Eubacterium Associated with Peritonitis
Several species of Eubacterium have been linked to complicated peritonitis, with Eubacterium rectale and Eubacterium limosum being the most frequently encountered. These species are capable of producing a variety of virulence factors, including toxins that exacerbate the inflammatory response and tissue damage in the abdomen.
Symptoms and Clinical Manifestations
The symptoms of complicated peritonitis due to Eubacterium are often severe and can rapidly worsen without appropriate treatment. Key symptoms include:
- Abdominal Pain: This is usually diffuse, severe, and worsens with movement or palpation.
- Fever: Elevated body temperature is a common sign of infection.
- Abdominal Distension: A noticeable bloating in the abdomen, often caused by the accumulation of gas and fluid in the peritoneal cavity.
- Nausea and Vomiting: These symptoms result from gastrointestinal involvement and increased intra-abdominal pressure.
- Signs of Sepsis: In more severe cases, patients may develop systemic inflammatory response syndrome (SIRS), leading to hypotension, tachycardia, and organ dysfunction.
Systemic Involvement and Complications
As the infection spreads, it can result in systemic complications such as:
- Sepsis: A life-threatening condition characterized by widespread inflammation and organ failure.
- Bacteremia: The presence of bacteria in the bloodstream, which can exacerbate the infection.
- Organ Dysfunction: This can include liver, kidney, and heart failure, requiring intensive care.
Diagnosis of Complicated Peritonitis Due to Eubacterium
Accurate diagnosis of complicated peritonitis due to Eubacterium is essential for effective treatment. Clinicians rely on a combination of clinical evaluation, imaging studies, and microbiological cultures to identify the pathogen and its associated complications.
Clinical Evaluation
The physician will assess the patient’s medical history and perform a thorough physical examination. Key indicators of peritonitis include:
- Tenderness upon palpation of the abdomen
- Guarding or rigidity, indicating muscle contraction in response to inflammation
- Positive signs of systemic infection, such as fever and elevated white blood cell count
Imaging Studies
Imaging techniques such as abdominal X-rays, ultrasound, and CT scans are crucial for evaluating the extent of peritoneal involvement. CT scans are particularly effective in identifying fluid collections, abscesses, and bowel perforations that may complicate peritonitis.
Microbiological Culture
Culturing peritoneal fluid obtained during diagnostic laparoscopy or paracentesis is essential for identifying the exact pathogen responsible for the infection. Cultures will help detect Eubacterium as well as other potential pathogens, guiding appropriate antibiotic therapy.
Treatment of Complicated Peritonitis Due to Eubacterium
The treatment of complicated peritonitis caused by Eubacterium requires a multifaceted approach, combining antimicrobial therapy with surgical intervention to address the source of infection.
Antibiotic Therapy
Effective antibiotic treatment is crucial for controlling Eubacterium infections. Since Eubacterium is anaerobic, it requires specific antibiotics that can target these bacteria. Commonly used antibiotics include:
- Metronidazole: A first-line treatment for anaerobic infections.
- Piperacillin-tazobactam: A broad-spectrum antibiotic effective against both anaerobic and aerobic pathogens.
- Carbapenems: In severe cases or when resistance is suspected.
Empiric therapy should be adjusted based on the results of microbiological cultures to ensure the correct antibiotics are used. Given the polymicrobial nature of these infections, combination therapy may be required to address both anaerobic and aerobic components.
Surgical Intervention
In addition to antibiotics, surgical intervention may be necessary to manage complicated peritonitis. Surgery is typically required to:
- Drain abscesses or fluid collections
- Repair bowel perforations or leaks
- Clean the peritoneal cavity to remove infected material
The type of surgery will depend on the underlying cause of the infection and the patient’s overall condition.
Prevention Strategies for Complicated Peritonitis
Preventing complicated peritonitis caused by Eubacterium largely revolves around minimizing the risk factors associated with peritoneal contamination. Strategies include:
- Prophylactic Antibiotics: Administering antibiotics prior to abdominal surgery can help prevent infection.
- Bowel Protection: Ensuring bowel integrity during surgery and promptly repairing any perforations can reduce the risk of bacterial contamination.
- Infection Control: Strict hygiene and aseptic techniques during medical procedures, including abdominal surgery and catheter placement, are essential to prevent peritoneal contamination.
Prognosis and Outcomes
The prognosis for patients with complicated peritonitis due to Eubacterium depends on the timeliness of diagnosis and treatment. Early recognition and intervention typically result in better outcomes, while delayed treatment increases the risk of sepsis and multi-organ failure. Mortality rates can be high, particularly in cases involving septic shock or significant organ dysfunction.