complicated e. coli uti (UTIs) are a prevalent health concern, with Escherichia coli (E. coli) being the primary causative agent. While many UTIs are straightforward and respond well to standard treatments, a subset is classified as complicated due to various factors that increase the risk of therapeutic failure. This article delves into the intricacies of complicated E. coli UTIs, examining their causes, risk factors, clinical manifestations, diagnostic approaches, treatment options, and preventive measures.
Understanding Complicated UTIs
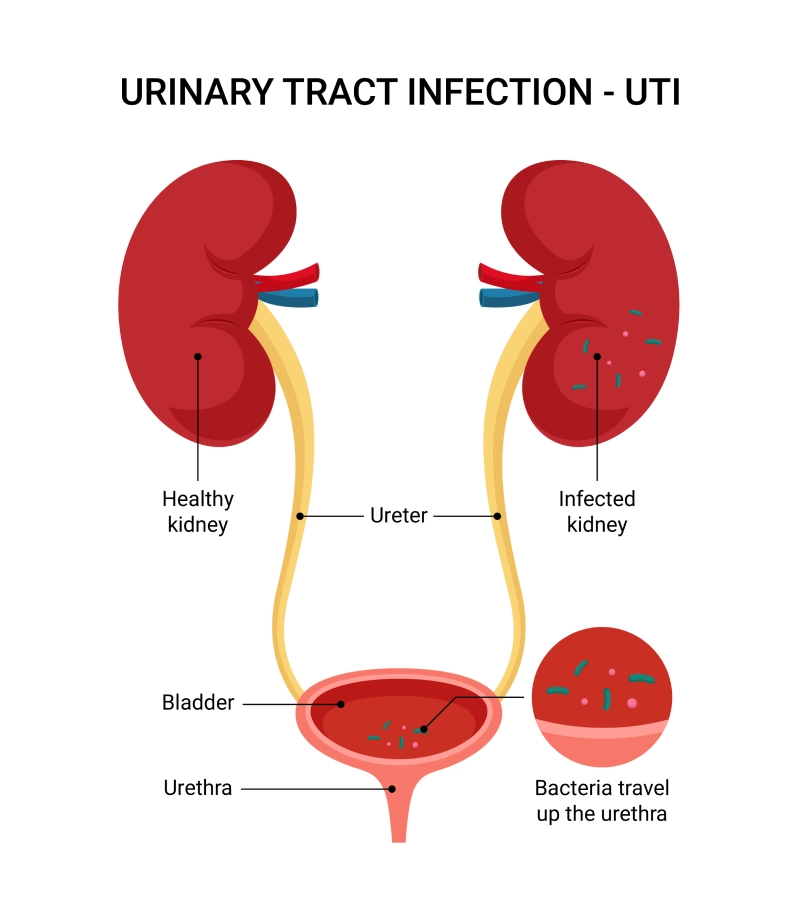
A UTI is deemed complicated when it is associated with conditions that heighten the risk of acquiring the infection or impede effective therapy. Such conditions include structural or functional abnormalities of the genitourinary tract, underlying diseases, or the presence of foreign bodies like catheters.
Etiology and Risk Factors
E. coli remains the predominant pathogen in both uncomplicated and complicated UTIs. However, in complicated cases, the spectrum of causative organisms broadens, and the prevalence of antibiotic-resistant strains, such as extended-spectrum β-lactamase (ESBL)-producing E. coli, increases.
Key risk factors for developing complicated E. coli UTIs include:
- Diabetes Mellitus: Impaired immune response and glycosuria can promote bacterial growth.
- Urinary Catheters: Indwelling catheters serve as a conduit for bacteria to enter the urinary tract.
- Urological Instrumentation: Procedures like cystoscopy or stent placements can introduce pathogens.
- Structural Abnormalities: Congenital anomalies or acquired conditions causing urinary stasis.
- Renal Calculi: Stones can harbor bacteria and obstruct urine flow.
Clinical Presentation
Patients with complicated E. coli UTIs may exhibit a range of symptoms, including:
- Fever and Chills: Indicative of systemic involvement.
- Dysuria: Painful urination is a common complaint.
- Flank Pain: Suggests upper urinary tract involvement.
- Hematuria: Presence of blood in the urine.
- Sepsis: In severe cases, systemic inflammatory response leading to septic shock.
Diagnostic Approaches
Accurate diagnosis is crucial for effective management. Recommended steps include:
- Urinalysis: Detection of pyuria, hematuria, and bacteriuria.
- Urine Culture: Identifies the causative organism and determines antibiotic susceptibility.
- Blood Cultures: Essential in febrile patients to check for bacteremia.
- Imaging Studies: Ultrasound or CT scans to identify structural abnormalities or abscesses.
Treatment Strategies
Management of complicated E. coli UTIs necessitates a comprehensive approach:
- Antibiotic Therapy: Empirical treatment should consider local resistance patterns. ESBL-producing E. coli may require carbapenems or other advanced antibiotics.
- Source Control: Addressing underlying issues such as removing or replacing catheters and relieving obstructions.
- Supportive Care: Ensuring adequate hydration and monitoring renal function.
Prevention Measures
Preventive strategies are vital to reduce the incidence of complicated UTIs:
- Catheter Management: Limit the use of indwelling catheters and adhere to aseptic techniques during insertion.
- Antibiotic Stewardship: Judicious use of antibiotics to minimize the development of resistant strains.
- Patient Education: Emphasize the importance of hydration, proper hygiene, and timely medical consultation for urinary symptoms.