Common Variable Agammaglobulinemia (CVA) is a primary immunodeficiency disorder characterized by a significant reduction or absence of immunoglobulins (antibodies) in the bloodstream. This condition leads to a weakened immune system, making affected individuals more vulnerable to recurrent infections, particularly those caused by bacteria. The disorder is often diagnosed in adolescence or adulthood, though symptoms can manifest earlier.
Understanding the underlying mechanisms, identifying the symptoms, and knowing the available treatments are crucial for managing CVA effectively.
Pathophysiology of Common Variable Agammaglobulinemia
CVA primarily affects the B cells, which are responsible for producing antibodies that fight off infections. In individuals with CVA, B cells either fail to mature properly or are unable to produce sufficient antibodies. This leads to low levels of all immunoglobulin classes (IgG, IgA, and IgM), which are essential for immune defense.
The condition is often caused by genetic mutations that affect immune cell signaling, particularly in genes involved in B-cell activation and differentiation. However, a definitive genetic cause remains elusive for many cases, and a combination of genetic and environmental factors may contribute to the development of the disorder.
Diagram: B-Cell Dysfunction in CVA (Mermaid Syntax)
mermaidCopyEditgraph LR
A[IgG, IgA, IgM Deficiency] --> B[B-Cell Dysfunction]
B --> C[B-Cell Maturation Impairment]
C --> D[Reduced Antibody Production]
D --> E[Increased Susceptibility to Infections]
Causes and Risk Factors of CVA
While the exact cause of CVA is not always clear, several factors have been associated with the condition:
- Genetic Mutations: In many cases, CVA is linked to mutations in genes responsible for immune cell development. Specific gene mutations, such as those in the CD19, CD20, or BTK genes, have been observed in some patients.
- Autoimmune Diseases: Individuals with CVA may also have an increased risk of developing autoimmune conditions, such as rheumatoid arthritis or lupus. The presence of these diseases suggests a complex interplay between the immune system and genetic predispositions.
- Environmental Factors: Though primarily a genetic disorder, environmental triggers like infections or exposure to toxins could play a role in the onset or exacerbation of CVA symptoms.
Symptoms of Common Variable Agammaglobulinemia
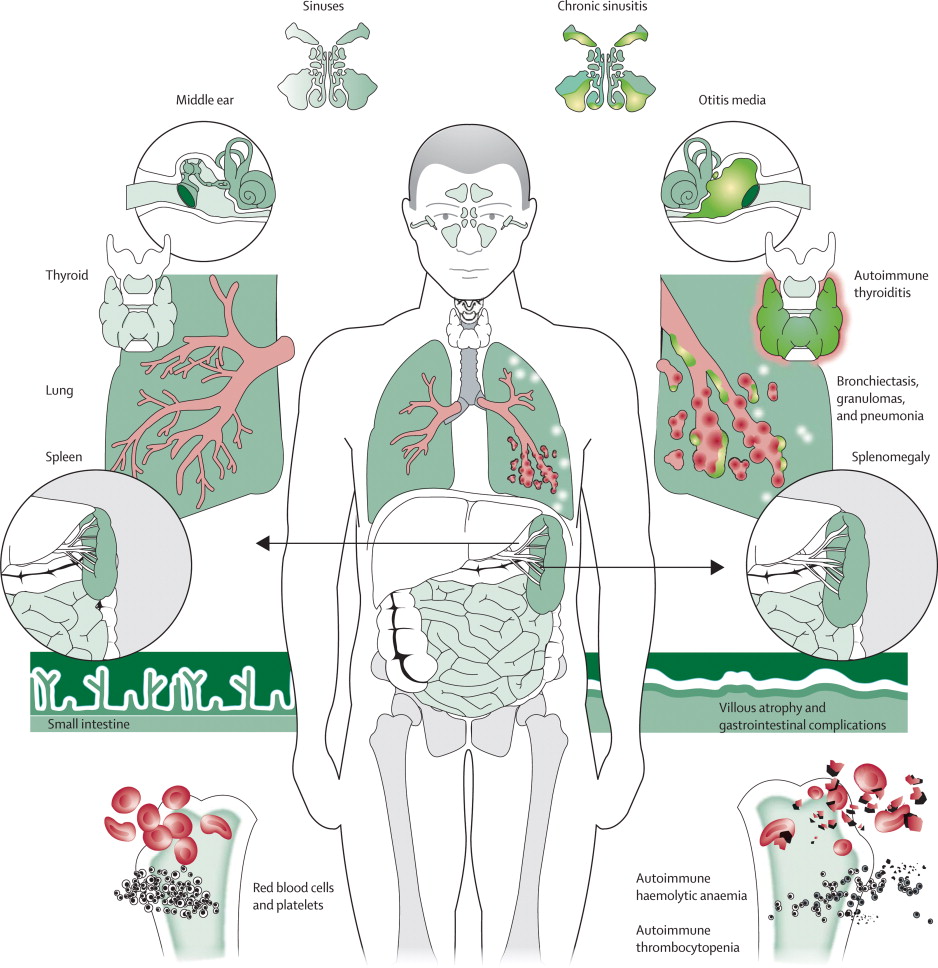
CVA manifests through a wide range of symptoms due to the body’s inability to produce antibodies. The most common symptoms include:
- Frequent Infections: Recurrent respiratory tract infections, sinusitis, pneumonia, and gastrointestinal infections are prevalent in those with CVA.
- Chronic Diarrhea: Gastrointestinal problems, including chronic diarrhea, are common due to the body’s impaired ability to fight off intestinal pathogens.
- Fatigue and Malaise: Due to ongoing infections and immune system dysfunction, individuals with CVA often report feeling persistently tired or unwell.
- Autoimmune Disorders: Some individuals may develop autoimmune diseases as a result of their compromised immune systems. These can include conditions like autoimmune thyroiditis and hemolytic anemia.
- Enlarged Lymph Nodes and Spleen: In response to persistent infections, some patients experience lymphadenopathy (enlarged lymph nodes) and splenomegaly (enlarged spleen).
Diagnosing Common Variable Agammaglobulinemia
Early diagnosis of CVA is essential to begin proper treatment and prevent complications. Several diagnostic tests are used to confirm the presence of CVA:
- Serum Immunoglobulin Levels: Blood tests reveal significantly low levels of immunoglobulins (IgG, IgA, and IgM).
- B-Cell Count: A flow cytometry test can measure B-cell count and functionality. In CVA patients, there is often an abnormal distribution of B cells.
- Genetic Testing: Although not always conclusive, genetic testing can help identify mutations in genes that are commonly associated with CVA.
- Infection History: A detailed medical history focusing on the frequency and type of infections is critical in the diagnostic process.
Treatment Options for CVA
While there is no cure for Common Variable Agammaglobulinemia, there are several treatment options that can help manage the condition and improve quality of life.
Immunoglobulin Replacement Therapy
The cornerstone of CVA treatment is immunoglobulin replacement therapy (IVIG or SCIG). This involves regular infusions or subcutaneous injections of immunoglobulins derived from blood donors. These immunoglobulins provide the missing antibodies, helping to reduce the frequency and severity of infections.
- Intravenous Immunoglobulin (IVIG): Administered through an IV, this therapy provides immediate relief and is typically given every 3-4 weeks.
- Subcutaneous Immunoglobulin (SCIG): For patients who prefer at-home treatments, SCIG is administered under the skin at regular intervals.
Antibiotic Prophylaxis
Since individuals with CVA are highly susceptible to infections, long-term antibiotic prophylaxis is often prescribed to prevent bacterial infections. Common antibiotics used include penicillin and azithromycin.
Supportive Care for Associated Complications
In addition to immunoglobulin therapy and antibiotics, patients with CVA may require additional treatments to manage complications such as autoimmune diseases, gastrointestinal issues, or organ dysfunction.
Stem Cell Transplantation
For individuals with severe forms of CVA or those who do not respond to conventional treatments, stem cell transplantation may be considered. This involves replacing dysfunctional bone marrow cells with healthy stem cells to restore normal immune function.
Prognosis and Quality of Life
With appropriate treatment, individuals with CVA can lead relatively normal lives. Immunoglobulin therapy significantly reduces the risk of infections and improves overall health. However, the disorder remains chronic, and patients require lifelong monitoring and treatment.
Although some patients may experience complications such as autoimmune diseases or organ damage, the majority of those diagnosed with CVA can live into adulthood and manage their symptoms effectively.