colorectal cancer, encompassing cancers of the colon and rectum, remains one of the leading causes of cancer-related mortality worldwide. Despite advancements in detection and treatment, understanding the nuances of this disease, including its risk factors, symptoms, diagnostic methods, and treatment strategies, is critical for improving outcomes and survival rates. In this comprehensive guide, we explore the various aspects of colorectal cancer to provide valuable insights for patients, healthcare providers, and the general public.
What is Colorectal Cancer?
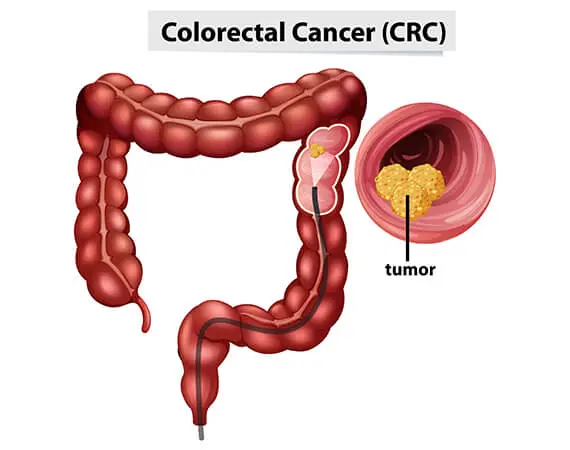
Colorectal cancer begins in the colon or rectum and typically develops from precancerous growths called polyps. Over time, these polyps can transform into malignant tumors. The colon is part of the digestive system, responsible for absorbing water and nutrients from food, while the rectum stores the body’s waste before elimination.
Risk Factors for Colorectal Cancer
Understanding the risk factors associated with colorectal cancer can aid in prevention and early detection. While some risk factors are uncontrollable, many can be managed through lifestyle changes.
1. Age
The majority of colorectal cancer cases occur in individuals over the age of 50, with risk increasing as individuals age. However, a growing number of younger adults are being diagnosed, highlighting the importance of early screening.
2. Family History
A family history of colorectal cancer significantly increases the risk, particularly if a first-degree relative was diagnosed before the age of 50. Inherited genetic mutations, such as Lynch syndrome and familial adenomatous polyposis (FAP), can also elevate risk.
3. Dietary Habits
A diet high in red or processed meats and low in fiber, fruits, and vegetables may increase the likelihood of developing colorectal cancer. Studies suggest that a diet rich in plant-based foods and low in unhealthy fats can help reduce this risk.
4. Physical Inactivity
Lack of regular physical activity has been linked to an increased risk of colorectal cancer. Exercise may help in maintaining a healthy weight and supporting proper bowel function, thereby lowering the risk.
5. Obesity
Obesity, particularly abdominal obesity, has been identified as a major risk factor for colorectal cancer. Obese individuals are more likely to develop polyps, which can lead to cancer.
6. Smoking and Alcohol Consumption
Both smoking and heavy alcohol consumption have been shown to increase the risk of colorectal cancer. These habits contribute to inflammation and DNA damage in the cells of the colon and rectum.
7. Personal Health History
Individuals with a history of inflammatory bowel diseases, such as Crohn’s disease or ulcerative colitis, are at a higher risk of colorectal cancer. Additionally, a personal history of colorectal polyps or other cancers can increase susceptibility.
Symptoms of Colorectal Cancer
Early stages of colorectal cancer often present with minimal or no symptoms. This is why routine screenings are crucial. As the disease progresses, however, various signs and symptoms may manifest:
- Persistent changes in bowel habits (e.g., diarrhea, constipation, or narrowing of stools)
- Blood in the stool or rectal bleeding
- Abdominal discomfort, such as cramps, gas, or bloating
- Unexplained weight loss or fatigue
- Feeling that the bowel does not empty completely
If any of these symptoms occur, especially in individuals at higher risk, it is vital to consult a healthcare provider for further evaluation.
Screening and Diagnosis
Early detection of colorectal cancer significantly improves the prognosis. The main diagnostic tools for colorectal cancer include:
1. Colonoscopy
The gold standard for colorectal cancer screening, colonoscopy allows physicians to visualize the entire colon and rectum to detect polyps or tumors. It is recommended for individuals over 50 or those at high risk due to family history or other factors.
2. Stool Tests
Fecal immunochemical tests (FIT) and guaiac-based fecal occult blood tests (FOBT) are used to detect hidden blood in the stool, which can indicate the presence of colorectal cancer or polyps. These tests are less invasive and can be performed at home, but they may require follow-up colonoscopy for confirmation.
3. CT Colonography
Also known as virtual colonoscopy, this imaging technique uses CT scans to create detailed images of the colon and rectum. It is an option for individuals who cannot undergo a traditional colonoscopy.
4. Biopsy
If a suspicious area is found during a colonoscopy or imaging study, a biopsy may be performed to collect a tissue sample for laboratory analysis. This is necessary to confirm the diagnosis of colorectal cancer.
Stages of Colorectal Cancer
The staging of colorectal cancer is crucial in determining the appropriate treatment plan. Stages are classified based on the extent of the cancer’s spread.
- Stage 0: Cancer is confined to the inner lining of the colon or rectum.
- Stage I: The tumor has grown into the layers of the colon or rectum but has not spread to lymph nodes or distant sites.
- Stage II: The cancer has spread through the wall of the colon or rectum but is still confined to the local area.
- Stage III: The cancer has spread to nearby lymph nodes but not to distant organs.
- Stage IV: The cancer has spread to distant organs, such as the liver or lungs.
Treatment Options for Colorectal Cancer
Treatment for colorectal cancer depends on the stage of the disease, the location of the tumor, and the patient’s overall health. Common treatment modalities include:
1. Surgery
Surgical resection is often the first line of treatment for colorectal cancer, particularly in early stages. The goal is to remove the tumor and any affected lymph nodes. In some cases, a portion of the colon or rectum may need to be removed, and a colostomy or ileostomy may be required.
2. Chemotherapy
Chemotherapy uses drugs to kill cancer cells or prevent their growth. It is commonly used after surgery to reduce the risk of recurrence, or for advanced-stage colorectal cancer to shrink tumors and alleviate symptoms.
3. Radiation Therapy
Radiation therapy uses high-energy beams to target cancer cells. It is more commonly used in rectal cancer, either before surgery to shrink the tumor or after surgery to eliminate remaining cancer cells.
4. Targeted Therapy and Immunotherapy
Targeted therapies aim to attack specific cancer cells while sparing normal cells. Immunotherapy helps the body’s immune system recognize and fight cancer cells. These therapies are often used in cases where the cancer has advanced or does not respond to conventional treatments.
5. Palliative Care
For advanced or metastatic colorectal cancer, palliative care is focused on improving quality of life and managing symptoms rather than attempting to cure the disease.
Prognosis and Survival Rates
The survival rate for colorectal cancer depends on the stage at diagnosis and the patient’s overall health. According to the American Cancer Society:
- Stage I: The five-year survival rate is approximately 90%.
- Stage II: The five-year survival rate is approximately 70-85%.
- Stage III: The five-year survival rate is approximately 50-70%.
- Stage IV: The five-year survival rate drops to approximately 10-15%.
Early detection through regular screenings is crucial for improving survival rates.
Prevention of Colorectal Cancer
While there is no surefire way to prevent colorectal cancer, several lifestyle modifications can help lower the risk:
- Regular Screening: Begin screening at age 50, or earlier if at high risk.
- Healthy Diet: Focus on a balanced diet rich in fruits, vegetables, and whole grains, while limiting red and processed meats.
- Physical Activity: Engage in regular physical activity to maintain a healthy weight and reduce the risk of obesity.
- Avoid Smoking and Excessive Alcohol: Limiting or avoiding smoking and alcohol consumption can significantly reduce the risk.
- Prophylactic Surgery: In high-risk individuals, preventive removal of polyps or even the colon may be considered.