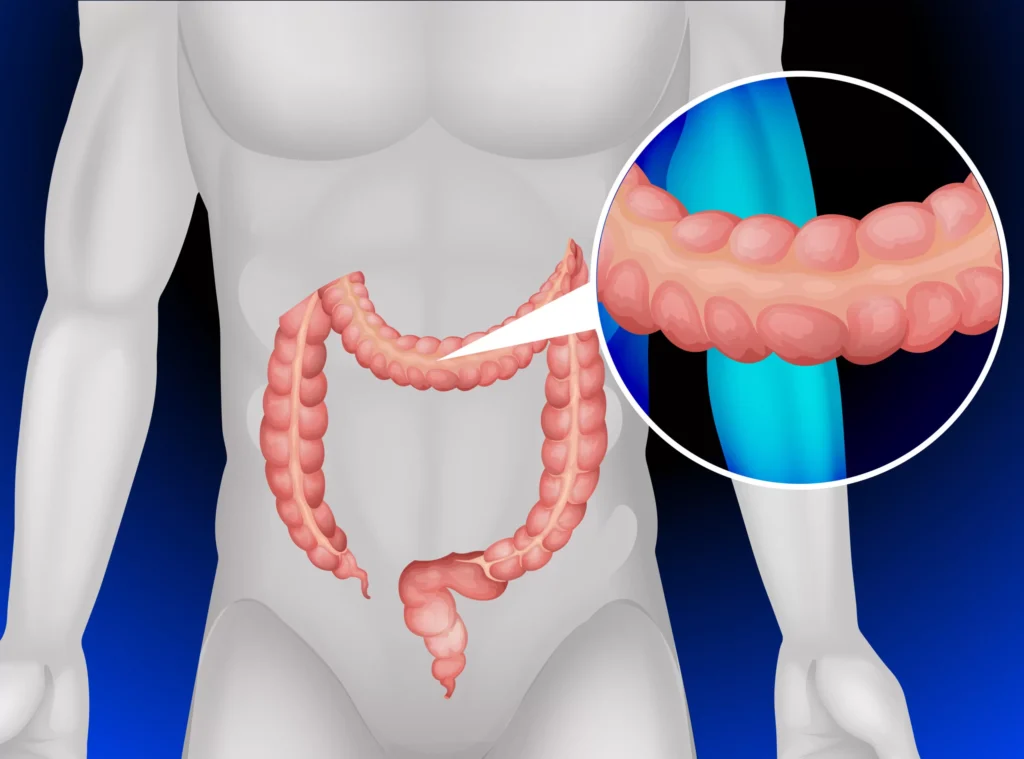
Collagenous colitis (CC) is a rare form of inflammatory bowel disease (IBD) that primarily affects the colon. It is characterized by chronic diarrhea and inflammation in the bowel, with the distinguishing feature of a thickened collagen layer found beneath the colon’s lining. This condition often goes undiagnosed due to its subtle symptoms and overlap with other gastrointestinal disorders. In this article, we delve deeply into collagenous colitis, covering its causes, symptoms, diagnosis, treatment options, and more.
What is Collagenous Colitis?
Collagenous colitis is a form of microscopic colitis, a group of disorders that cause inflammation in the colon and lead to chronic watery diarrhea. While the exact cause remains unclear, studies suggest a combination of genetic predisposition, immune system dysfunction, and environmental factors may contribute to its development. This condition is often diagnosed through biopsies and imaging tests, as it typically does not manifest visible symptoms during routine endoscopic procedures.
Unlike other forms of colitis, collagenous colitis is marked by an increased amount of collagen beneath the epithelial cells of the colon, causing inflammation that disrupts normal bowel function.
Causes
Although the precise cause of collagenous colitis is unknown, several factors have been identified as potential contributors to the condition:
- Immune System Dysfunction:
One theory is that the immune system mistakenly attacks the cells of the colon, leading to inflammation and the buildup of collagen fibers beneath the mucosal layer. This immune-mediated process may be triggered by infections, environmental toxins, or genetic predisposition. - Genetics:
There is evidence suggesting that a family history of inflammatory bowel disease or autoimmune disorders can increase the risk of developing collagenous colitis. Certain genetic markers have been linked to a predisposition to this condition. - Medications:
Some medications, particularly nonsteroidal anti-inflammatory drugs (NSAIDs), proton pump inhibitors (PPIs), and certain antibiotics, have been associated with an increased risk of developing microscopic colitis, including collagenous colitis. - Infections and Environmental Factors:
Bacterial or viral infections may also play a role in triggering or exacerbating collagenous colitis, although more research is needed to fully understand these connections.
Symptoms
The hallmark symptom of collagenous colitis is chronic watery diarrhea, which can last for weeks or even months. Other symptoms may include:
- Abdominal pain or discomfort
- Cramping
- Weight loss
- Fatigue
- Occasional blood or mucus in stool (though this is less common)
- Nausea
Symptoms of collagenous colitis can vary in severity from mild to debilitating, and some individuals may experience periods of flare-ups followed by remission. The condition is often mistaken for irritable bowel syndrome (IBS) or other gastrointestinal disorders due to the overlap in symptoms.
Diagnosis
Diagnosing collagenous colitis can be challenging, as its symptoms overlap with those of other gastrointestinal disorders, including IBS, inflammatory bowel disease (IBD), and infections. Typically, a combination of medical history review, laboratory tests, and imaging techniques are used to confirm the diagnosis.
Colonoscopy and Biopsy
A colonoscopy is a key diagnostic tool for collagenous colitis. During the procedure, a thin, flexible tube with a camera is inserted into the colon to visualize any abnormalities. However, in most cases, no significant changes will be visible during the colonoscopy. This is why a biopsy (a small tissue sample) is required to confirm the diagnosis. Under a microscope, the biopsy will reveal an abnormal increase in collagen deposits beneath the colon lining, which is characteristic of collagenous colitis.
Blood Tests and Stool Analysis
Blood tests may be conducted to check for signs of inflammation or infection, while stool samples can help rule out other conditions such as infections, parasites, or other types of colitis.
Treatment Options
While there is no cure for collagenous colitis, several treatment options are available to help manage symptoms and improve quality of life. The goal of treatment is to reduce inflammation, control diarrhea, and prevent flare-ups.
Medications
- Anti-inflammatory Drugs:
Medications such as mesalamine (5-aminosalicylic acid) are often prescribed to reduce inflammation in the colon and manage symptoms. - Immunosuppressants:
In cases where anti-inflammatory drugs are not effective, immunosuppressive medications like azathioprine or methotrexate may be prescribed. These drugs work by suppressing the immune system’s activity to prevent further inflammation. - Corticosteroids:
For more severe cases of collagenous colitis, corticosteroids may be used to quickly reduce inflammation and manage symptoms. However, they are typically not recommended for long-term use due to potential side effects. - Antidiarrheal Medications:
Medications like loperamide may be used to control diarrhea during flare-ups. These should be used with caution and under a healthcare provider’s supervision. - Bile Acid Sequestrants:
Some individuals with collagenous colitis benefit from bile acid sequestrants, which help regulate the flow of bile and reduce diarrhea.
Dietary Modifications
Adopting a low-fat, high-fiber diet may help some individuals manage their symptoms. It’s important to stay hydrated due to the frequent diarrhea. In some cases, an elimination diet may be used to identify specific foods that trigger flare-ups.
Probiotics and Supplements
Probiotics may help restore a healthy balance of gut bacteria, potentially alleviating some symptoms. Additionally, vitamin and mineral supplements may be recommended to prevent deficiencies, especially if diarrhea is chronic.
Prognosis and Living
While collagenous colitis is a chronic condition, many individuals can manage their symptoms with the right combination of treatments and lifestyle adjustments. The severity of the disease varies from person to person, with some experiencing mild symptoms and others facing more debilitating effects. Regular follow-up visits with a healthcare provider are essential for monitoring the condition and adjusting treatment as needed.
Preventing Flare-Ups
To prevent flare-ups, individuals with collagenous colitis should focus on managing stress, avoiding triggers (such as certain medications or foods), and following their treatment plan. Staying informed about the condition and its progression is crucial for maintaining good bowel health.