Acute Intestinal Amebiasis Due to Entamoeba Histolytica, a protozoan parasite, is the causative agent of acute intestinal amebiasis, a condition affecting millions globally. This pathogen thrives in regions with inadequate sanitation, transmitting via the fecal-oral route through ingestion of cysts in contaminated food or water. Distinct from non-pathogenic amoebae like Entamoeba dispar, E. histolytica invades intestinal tissues, leading to severe clinical manifestations.
Pathophysiology and Lifecycle of Entamoeba Histolytica
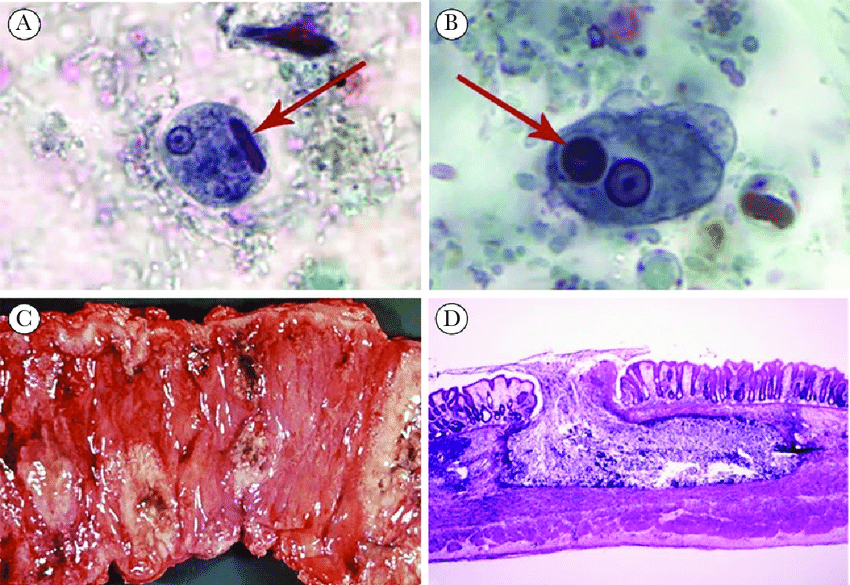
The lifecycle comprises two stages: infectious cysts and invasive trophozoites. Upon cyst ingestion, excystation occurs in the small intestine, releasing trophozoites that colonize the colon. Trophozoites penetrate mucosal barriers via cysteine proteinases, causing flask-shaped ulcers. Subsequent encystation in the lumen allows cyst excretion, perpetuating transmission.
Clinical Presentation of Acute Intestinal Amebiasis Due to Entamoeba Histolytica
Symptomatology ranges from asymptomatic carriage to severe dysentery. Key manifestations include:
- Amebic Dysentery: Bloody, mucoid diarrhea with abdominal cramping.
- Fulminant Colitis: Rare but life-threatening, featuring toxic megacolon or perforation.
- Chronic Infection: Recurrent diarrhea and weight loss.
Extraintestinal complications, such as hepatic abscesses, arise from hematogenous spread.
Diagnostic Approaches for Acute Intestinal Amebiasis Due to Entamoeba Histolytica
Accurate diagnosis hinges on integrating clinical, microbiological, and imaging data:
- Stool Antigen Testing: Detects E. histolytica-specific proteins, offering high sensitivity.
- PCR: Confirms species differentiation, critical for distinguishing pathogenic strains.
- Serology: Identifies antibodies in invasive cases; useful for extraintestinal diagnoses.
- Colonoscopy: Reveals characteristic ulcers, with biopsies enabling histopathological confirmation.
Therapeutic Strategies for Amebic Dysentery
First-line treatment involves nitroimidazoles (e.g., metronidazole) to eradicate invasive trophozoites, followed by luminal agents (paromomycin or diloxanide furoate) to eliminate cysts. Supportive care includes rehydration and electrolyte management. For hepatic abscesses, prolonged antimicrobial therapy combined with drainage (if >10 cm) is recommended.
Complications and Prognosis
Untreated cases risk colonic perforation, peritonitis, or systemic dissemination. Hepatic abscesses, though treatable, may rupture into pleural or peritoneal cavities. Mortality remains low (<1%) with timely intervention but escalates in immunocompromised individuals.
Prevention and Control Measures
Effective prevention relies on:
- Sanitation Infrastructure: Access to clean water and sewage disposal.
- Health Education: Promoting hand hygiene and safe food practices.
- Screening Programs: Identifying asymptomatic carriers in endemic zones.
Acute Intestinal Amebiasis Due to Entamoeba Histolytica (Acute intestinal amebiasis) demands a multifaceted approach encompassing early diagnosis, targeted therapy, and robust public health initiatives. By prioritizing these strategies, we mitigate the global burden of Entamoeba histolytica infections, safeguarding vulnerable populations from this pervasive parasitic threat.