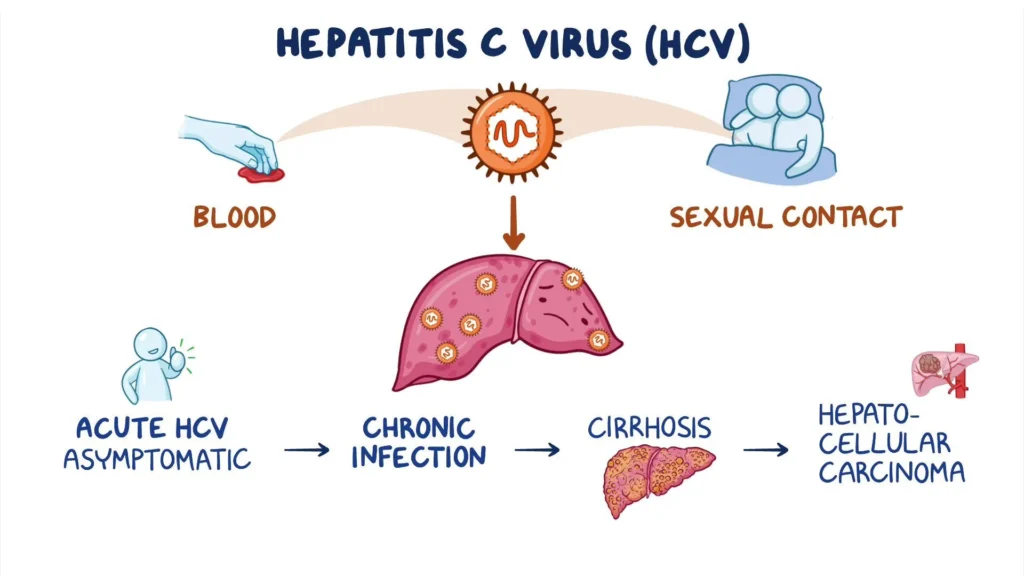
Acute hepatitis C is a viral liver infection caused by the hepatitis C virus (HCV). It is often asymptomatic but can lead to chronic infection if left untreated. This condition is a significant global health concern due to its potential to cause severe liver complications, including cirrhosis and liver cancer. Early detection and appropriate medical intervention are crucial for managing the disease effectively.
Transmission and Risk Factors
Hepatitis C is primarily spread through blood-to-blood contact. The most common transmission routes include:
- Intravenous Drug Use: Sharing contaminated needles is the leading cause of HCV transmission.
- Blood Transfusions (Before 1992): Prior to improved screening protocols, blood transfusions posed a high risk.
- Unsafe Medical Practices: Poor sterilization of medical equipment can facilitate the spread of HCV.
- Unprotected Sexual Contact: Though less common, HCV can be transmitted through sexual activity, particularly among individuals with multiple partners or co-existing sexually transmitted infections.
- Mother-to-Child Transmission: Perinatal transmission occurs when an infected mother passes the virus to her baby during childbirth.
Symptoms of Acute Hepatitis C
Many individuals with acute hepatitis C remain asymptomatic. However, those who develop symptoms may experience:
- Fatigue
- Jaundice (Yellowing of the Skin and Eyes)
- Dark Urine and Pale Stools
- Abdominal Pain (Especially in the Upper Right Quadrant)
- Nausea and Vomiting
- Loss of Appetite
- Fever
- Joint Pain
Diagnosis of Acute Hepatitis C
Timely diagnosis is critical for managing acute hepatitis C and preventing its progression to chronic infection. Diagnostic methods include:
- HCV Antibody Test: Detects the presence of antibodies indicating HCV exposure.
- HCV RNA Test (PCR Test): Confirms active infection by detecting viral RNA.
- Liver Function Tests (LFTs): Measures levels of liver enzymes (ALT and AST) to assess liver inflammation.
- FibroScan or Liver Biopsy: Determines the extent of liver damage in severe cases.
Pathogenesis of Hepatitis C
HCV primarily targets hepatocytes, leading to liver inflammation and fibrosis.
Treatment and Management
1. Antiviral Therapy
- Direct-Acting Antivirals (DAAs): Highly effective in clearing the virus within 8–12 weeks.
- Interferon-Based Therapy (Less common): Previously used but now largely replaced by DAAs due to their higher efficacy and fewer side effects.
2. Supportive Care
- Adequate Hydration and Nutrition
- Avoiding Alcohol and Hepatotoxic Drugs
- Regular Liver Function Monitoring
3. Preventive Measures
- Safe Injection Practices
- Blood Screening for Donors
- Education on HCV Transmission Risks
Prognosis and Long-Term Outlook
While some individuals clear the virus naturally, around 75–85% develop chronic hepatitis C, increasing the risk of liver complications. With early treatment using DAAs, over 95% of cases achieve a sustained virologic response (SVR), effectively curing the infection.
Acute hepatitis C remains a significant public health issue. Early diagnosis and prompt treatment with direct-acting antivirals can prevent chronic complications, ensuring better patient outcomes. Preventive measures, including safe injection practices and blood donor screening, play a crucial role in reducing transmission rates.