Absence epilepsy with multiple seizure types is a complex neurological disorder characterized by frequent absence seizures alongside other types of epileptic episodes. This condition typically affects children and adolescents, though it can persist or evolve into adulthood. Understanding the underlying mechanisms, symptoms, and treatment approaches is critical for managing this multifaceted condition effectively.
What is Absence Epilepsy?
Absence epilepsy, also known as petit mal epilepsy, is a form of generalized epilepsy primarily characterized by brief, sudden lapses in consciousness. These episodes, referred to as absence seizures, are often mistaken for daydreaming or inattention. In cases involving multiple seizure types, patients may also experience tonic-clonic seizures, myoclonic seizures, or atonic seizures, making diagnosis and management more complex.
Key Features of Absence Epilepsy
- Duration of Absence Seizures: Typically last 5–20 seconds, occurring multiple times per day.
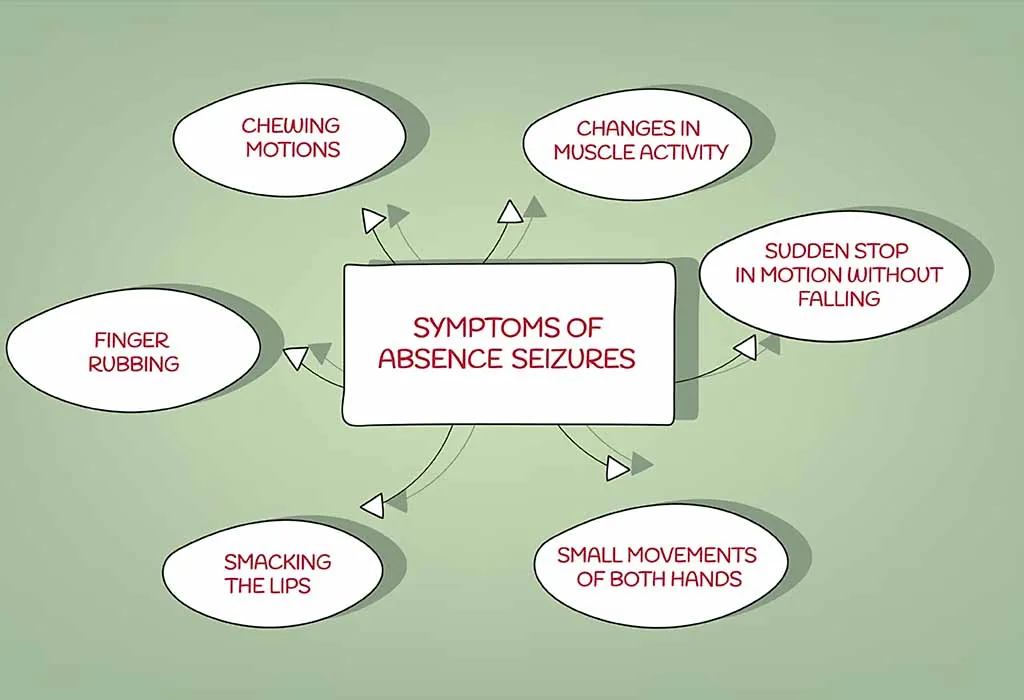
- Symptoms: Sudden cessation of activity, staring episodes, blinking, or subtle movements like lip-smacking.
- Onset Age: Most commonly manifests between 4–12 years of age.
Types of Seizures in Absence Epilepsy with Multiple Seizure Types
1. Absence Seizures
These are the hallmark seizures in absence epilepsy. They are characterized by:
- Brief loss of awareness.
- No post-ictal confusion or recovery phase.
- Sudden onset and termination.
2. Tonic-Clonic Seizures
Tonic-clonic seizures involve two distinct phases:
- Tonic Phase: Stiffening of muscles, often causing the person to fall.
- Clonic Phase: Rhythmic jerking of limbs and facial muscles.
3. Myoclonic Seizures
Myoclonic seizures involve sudden, brief jerking movements, often affecting the upper body. These seizures can occur in clusters and may be triggered by specific factors like sleep deprivation or flashing lights.
4. Atonic Seizures
Atonic seizures, also known as drop attacks, result in sudden loss of muscle tone, causing the individual to collapse. These episodes can lead to injuries if protective measures are not in place.
Pathophysiology of Absence Epilepsy
Absence seizures result from abnormal electrical activity in the brain, particularly involving the thalamocortical circuitry. This misfiring leads to a synchronized spike-and-wave discharge pattern on an electroencephalogram (EEG), typically at 3 Hz. When combined with other seizure types, the underlying mechanisms may involve broader neuronal networks, complicating the condition further.
Causes and Risk Factors
Genetic Influences
- Heritability: Strong genetic predisposition, often associated with specific gene mutations such as those in the CACNA1A or GABRG2 genes.
- Family History: Individuals with a family history of epilepsy are at a higher risk.
Environmental Triggers
- Stress: Emotional or physical stress can precipitate seizures.
- Sleep Deprivation: Lack of adequate rest is a common trigger.
- Photosensitivity: Flashing lights or patterns can provoke seizures in susceptible individuals.
Diagnosing Absence Epilepsy with Multiple Seizure Types
A thorough diagnostic process is essential to distinguish this condition from other epilepsy syndromes.
1. Electroencephalogram (EEG)
An EEG is the gold standard for diagnosing absence epilepsy. The characteristic 3 Hz spike-and-wave pattern is typically observed during absence seizures, whereas other seizure types may present distinct EEG signatures.
2. Neuroimaging
Magnetic Resonance Imaging (MRI) may be employed to rule out structural abnormalities that could contribute to seizures.
3. Clinical Evaluation
A detailed history of the patient’s seizure episodes, including frequency, duration, and associated symptoms, is critical for accurate diagnosis.
Treatment Approaches
Managing absence epilepsy with multiple seizure types requires a tailored approach, often combining pharmacologic therapies with lifestyle modifications and supportive care.
Pharmacologic Treatments
1. Ethosuximide
- First-line treatment for absence seizures.
- Effective in reducing the frequency of absence episodes without significant sedative effects.
2. Valproate
- Broad-spectrum efficacy for multiple seizure types.
- Requires careful monitoring due to potential side effects, including hepatotoxicity.
3. Lamotrigine
- Useful for both absence and tonic-clonic seizures.
- Fewer cognitive side effects compared to other antiepileptic drugs.
4. Levetiracetam
- Often prescribed for adjunctive treatment in myoclonic and tonic-clonic seizures.
Non-Pharmacologic Therapies
1. Ketogenic Diet
A high-fat, low-carbohydrate diet has been shown to reduce seizure frequency in drug-resistant cases.
2. Vagus Nerve Stimulation (VNS)
VNS therapy involves implanting a device to stimulate the vagus nerve, which can help control seizures.
3. Lifestyle Modifications
- Ensuring regular sleep patterns.
- Avoiding known triggers, such as flashing lights or high-stress environments.
Prognosis and Long-Term Management
The prognosis for absence epilepsy with multiple seizure types varies depending on the individual’s response to treatment and the severity of their condition. Many children with absence epilepsy achieve remission during adolescence, but the presence of additional seizure types may necessitate ongoing management into adulthood.
Importance of Regular Follow-Ups
Patients should undergo regular follow-ups with a neurologist to adjust treatment plans and monitor for potential side effects of medications.
Absence epilepsy with multiple seizure types presents unique challenges requiring a comprehensive approach to diagnosis and treatment. By combining pharmacologic therapies, lifestyle adjustments, and advanced interventions, healthcare providers can effectively manage this condition and improve the quality of life for patients. Early intervention, regular monitoring, and individualized care plans are critical to ensuring optimal outcomes.