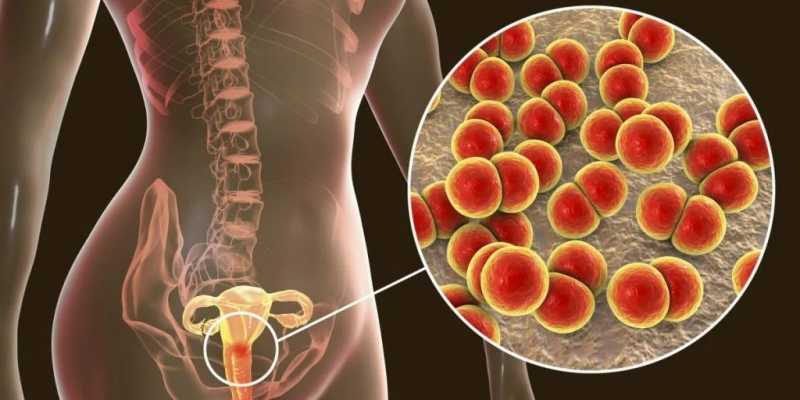
Pelvic Inflammatory Disease (PID) represents a spectrum of inflammatory disorders affecting the upper female genital tract, including the uterus, fallopian tubes, and ovaries. While commonly associated with sexually transmitted infections like Neisseria gonorrhoeae and Chlamydia trachomatis, anaerobic bacteria, notably Clostridium species, have emerged as significant yet rare pathogens in PID cases. This article delves into the role of Clostridium species in PID, emphasizing Clostridium perfringens and Clostridium sordellii, their pathogenesis, clinical manifestations, diagnostic approaches, treatment modalities, and preventive measures.
The Role of Clostridium Species in PID
Pathogenesis
Clostridium species are Gram-positive, spore-forming anaerobes ubiquitously present in the environment and the human gastrointestinal tract. Their involvement in gynecological infections, particularly PID, is uncommon but can lead to severe outcomes. The pathogenicity of Clostridium in PID is primarily attributed to toxin production, which can cause extensive tissue necrosis and systemic toxicity.
Clinical Manifestations
Infections caused by Clostridium species in the pelvic region can present with:
- Severe lower abdominal pain: Often acute in onset.
- Fever and chills: Indicative of systemic involvement.
- Malodorous vaginal discharge: Suggestive of anaerobic bacterial activity.
- Tachycardia and hypotension: Signs of systemic toxicity or toxic shock syndrome.
A notable case involved a 22-year-old woman who presented with right lower abdominal pain, initially suspected as appendicitis. Surgical findings revealed turbid fluid and inflamed, dilated fallopian tubes, leading to a diagnosis of PID. Cultures identified Clostridium perfringens, and the patient developed toxic shock syndrome, underscoring the severity of such infections.
Diagnostic Approaches
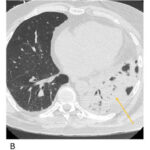
Accurate and prompt diagnosis of Clostridium-associated PID is crucial due to its rapid progression and potential for severe complications. Diagnostic strategies include:
- Clinical Evaluation: Assessment of symptoms such as lower abdominal pain, fever, and abnormal vaginal discharge.
- Imaging Studies: Ultrasound or CT scans may reveal pelvic abscesses or tubo-ovarian complexes.
- Microbiological Cultures: Isolation of Clostridium species from pelvic or peritoneal fluid samples confirms the diagnosis.
- Laboratory Tests: Elevated white blood cell count, C-reactive protein, and erythrocyte sedimentation rate may indicate infection.
Treatment Modalities
Management of Clostridium-associated PID involves:
- Antibiotic Therapy: Empirical broad-spectrum antibiotics should be initiated promptly, targeting both aerobic and anaerobic organisms. Once Clostridium is identified, therapy should include agents effective against anaerobes, such as clindamycin or metronidazole, combined with agents like penicillin or third-generation cephalosporins to cover other potential pathogens. pubmed.ncbi.nlm.nih.gov
- Surgical Intervention: In cases of abscess formation or failure of medical therapy, surgical drainage or debridement may be necessary.
- Supportive Care: Monitoring and managing systemic symptoms, including fluid resuscitation and hemodynamic support in cases of toxic shock syndrome.
Prevention Strategies
Preventive measures to reduce the risk of Clostridium-associated PID include:
- Safe Sexual Practices: Consistent use of condoms and limiting the number of sexual partners to reduce the risk of sexually transmitted infections.
- Regular Medical Check-Ups: Routine gynecological examinations and prompt treatment of any infections.
- Avoidance of Unnecessary Douching: Douching can disrupt the normal vaginal flora, potentially facilitating the overgrowth of pathogenic bacteria.