Endometritis, the inflammation of the endometrial lining of the uterus, is a significant gynecological condition that can lead to severe reproductive complications if not promptly addressed. Among the various pathogens implicated in its etiology, certain species of the genus Clostridium have garnered attention due to their association with both acute and chronic forms of the disease. This article delves into the role of Clostridium species in endometritis, exploring their pathogenesis, clinical manifestations, diagnostic methodologies, and therapeutic interventions.
Pathogenesis of Clostridium in Endometritis
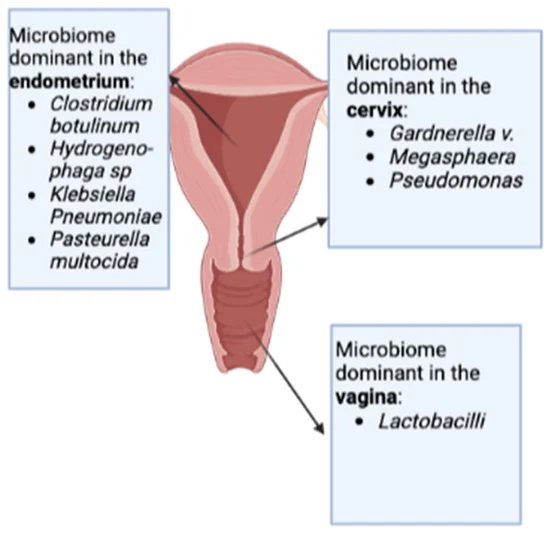
Clostridium species are Gram-positive, obligate anaerobic bacilli capable of forming spores, which confer resilience in adverse environmental conditions. In the context of endometritis, species such as Clostridium butyricum, Clostridium sordellii, Clostridium perfringens, and Clostridium bifermentans have been identified as causative agents. These bacteria can colonize the uterine cavity, especially following obstetric procedures or gynecological interventions that disrupt the endometrial barrier.
The pathogenicity of Clostridium species in the uterus is primarily attributed to their toxin-producing capabilities. For instance, C. sordellii produces lethal toxins that can lead to toxic shock syndrome, characterized by rapid clinical deterioration. Similarly, C. perfringens is known for its alpha toxin, which can cause gas gangrene and severe uterine infections. The anaerobic environment of the uterine cavity post-infection provides an ideal milieu for the proliferation of these pathogens, leading to tissue necrosis and systemic toxicity.
Clinical Manifestations
The clinical presentation of clostridial endometritis can vary from mild to severe and is often rapid in onset. Common symptoms include:
- Fever: Elevated body temperature often exceeding 38°C.
- Abdominal Pain: Severe lower abdominal or pelvic pain.
- Vaginal Discharge: Foul-smelling, purulent discharge.
- Tachycardia: Increased heart rate.
- Hypotension: Low blood pressure, indicative of systemic involvement.
In severe cases, patients may develop signs of septic shock, including multi-organ failure and disseminated intravascular coagulation. Notably, infections caused by C. sordellii may present with minimal fever but profound leukocytosis and capillary leak syndrome, leading to rapid hemodynamic collapse.
Diagnostic Approaches
Accurate and timely diagnosis of clostridial endometritis is crucial for effective management. Diagnostic strategies encompass:
- Microbiological Cultures: Isolation of Clostridium species from endometrial or vaginal specimens under anaerobic conditions.
- Molecular Techniques: Polymerase chain reaction (PCR) assays targeting specific clostridial DNA sequences enhance detection sensitivity.
- Imaging Studies: Ultrasonography or computed tomography (CT) scans may reveal uterine enlargement, gas formation within the endometrium, or abscess formation.
- Histopathological Examination: Biopsy samples can demonstrate necrosis, inflammation, and the presence of Gram-positive bacilli.
Given the rapid progression associated with clostridial infections, a high index of suspicion is necessary, especially in postpartum women or those with recent uterine instrumentation presenting with compatible symptoms.
Therapeutic Strategies
Management of clostridial endometritis involves a combination of antimicrobial therapy, surgical intervention, and supportive care:
- Antibiotic Therapy: Empirical broad-spectrum antibiotics should be initiated promptly, with subsequent tailoring based on culture sensitivities. Agents effective against Clostridium species include penicillin, metronidazole, and clindamycin.
- Surgical Intervention: In cases of abscess formation, necrotic tissue, or lack of response to medical therapy, surgical procedures such as dilation and curettage or hysterectomy may be warranted.
- Supportive Care: Hemodynamic stabilization, fluid resuscitation, and management of organ dysfunction are critical components of care in severe cases.
Recent studies have explored the role of probiotics in mitigating endometrial inflammation. For instance, Clostridium butyricum has demonstrated protective effects against Escherichia coli-induced endometritis in murine models by modulating the NF-κB signaling pathway and enhancing the endometrial barrier function.