Osteomyelitis, a serious infection of the bone, can be caused by various bacterial species, including Citrobacter. Citrobacter osteomyelitis, though rare, presents unique challenges in diagnosis and management due to its distinct pathogenic profile and resistance patterns. This article explores the causes, clinical features, diagnostic approach, treatment options, and preventive measures for Citrobacter osteomyelitis.
Understanding Citrobacter and Its Role in Osteomyelitis
What Is Citrobacter?
Citrobacter is a genus of Gram-negative, facultative anaerobic bacteria belonging to the Enterobacteriaceae family. These organisms are commonly found in the environment, including soil, water, and human gastrointestinal tracts. While Citrobacter species, such as Citrobacter freundii and Citrobacter koseri, are typically opportunistic pathogens, they can cause serious infections in immunocompromised individuals.
Pathogenesis in Osteomyelitis
In osteomyelitis, Citrobacter species invade bone tissue, either directly through trauma, surgery, or contiguous infection from nearby tissues, or hematogenously via the bloodstream. Risk factors include diabetes, immunosuppression, and invasive procedures.
Clinical Presentation
Common Symptoms
Patients with Citrobacter osteomyelitis may exhibit:
- Localized bone pain and tenderness
- Swelling and redness over the affected area
- Fever and chills (in systemic cases)
- Reduced range of motion in nearby joints
Chronic vs. Acute Presentation
Presents with rapid symptom onset, while chronic cases may have insidious symptoms, including draining sinus tracts and non-healing wounds.
Diagnosis
Clinical Evaluation
A thorough medical history and physical examination are essential. Clinicians should inquire about recent surgeries, trauma, and underlying health conditions.
Laboratory Tests
- Blood Tests: Elevated white blood cell (WBC) count, C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR) may indicate infection.
- Blood Cultures: Essential for identifying the causative organism.
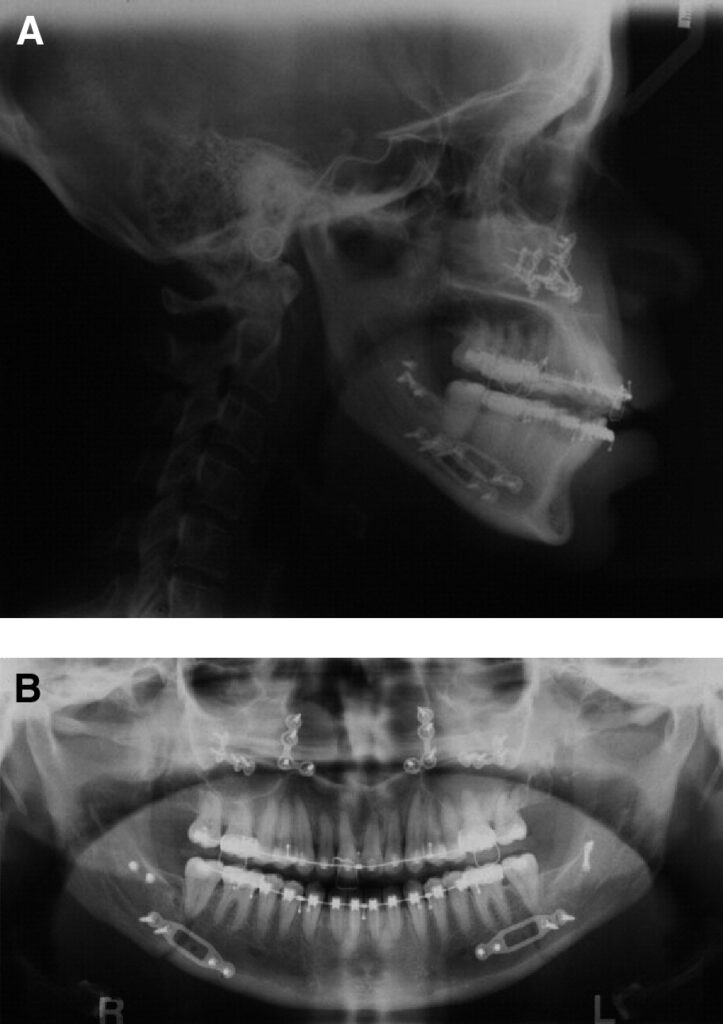
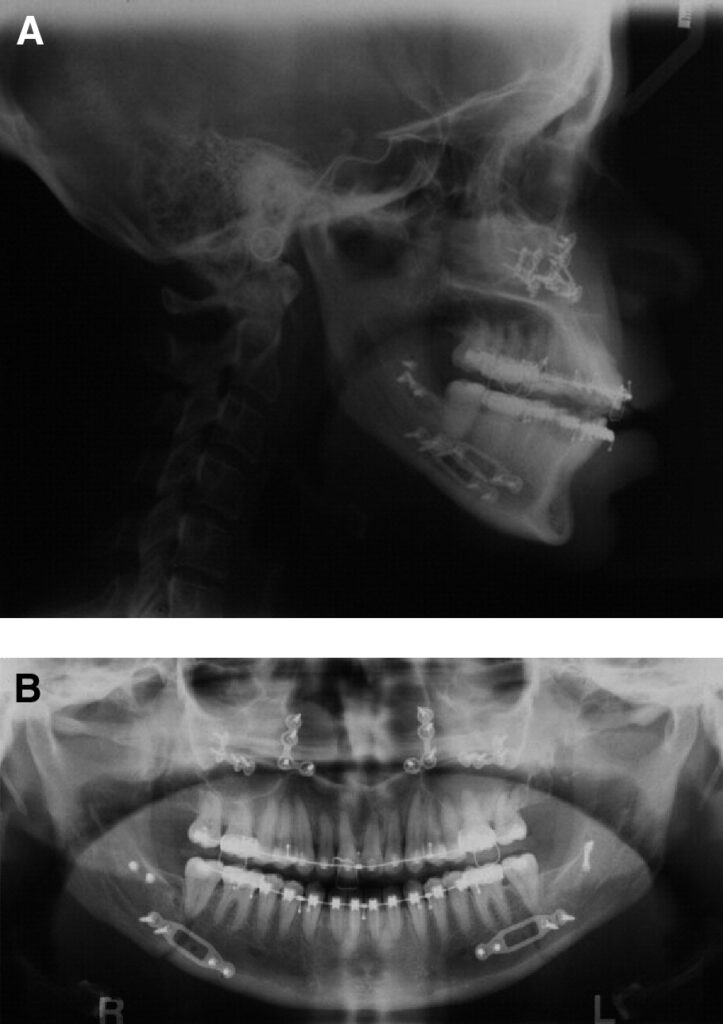
Imaging Studies
- X-rays: Useful for detecting bone destruction in advanced stages.
- MRI: Highly sensitive for early detection of bone and soft tissue involvement.
- CT Scans: Useful for surgical planning.
Microbiological Analysis
Bone biopsy and culture remain the gold standard for confirming Citrobacter osteomyelitis and determining antibiotic susceptibility.
Treatment
Antibiotic Therapy
Treatment begins with empirical broad-spectrum antibiotics, tailored based on culture results. Citrobacter species often display resistance to multiple antibiotics, necessitating careful selection. Commonly used agents include:
- Third-generation cephalosporins (e.g., ceftriaxone)
- Carbapenems (e.g., meropenem)
- Fluoroquinolones (e.g., ciprofloxacin)
Therapy typically lasts 4-6 weeks, with intravenous administration in the initial phase.
Surgical Intervention
Surgical management may be required to:
- Debride necrotic bone and tissue
- Drain abscesses
- Stabilize the affected bone using orthopedic implants
Supportive Care
Pain management, nutritional support, and management of underlying conditions (e.g., diabetes) are crucial for optimal recovery.
Prevention
Reducing Risk Factors
- Infection Control: Adhere to strict aseptic techniques during surgeries.
- Chronic Disease Management: Optimize control of diabetes and other comorbidities.
- Early Treatment: Promptly address soft tissue infections to prevent spread.
Prophylactic Measures
Prophylactic antibiotics may be considered for high-risk surgical procedures to minimize the risk of postoperative osteomyelitis.
Prognosis
The prognosis for Citrobacter osteomyelitis depends on timely diagnosis and treatment. While chronic cases may pose challenges due to recurrence or antibiotic resistance, early and aggressive management often leads to favorable outcomes.