A complicated urinary tract infection (UTI) caused by Citrobacter species represents a significant medical concern, especially due to its association with more severe infections that often require comprehensive management. This article delves into the critical aspects of Citrobacter complicated UTIs, including symptoms, causes, diagnosis, treatment, and prevention.
What Is Citrobacter Complicated UTI?
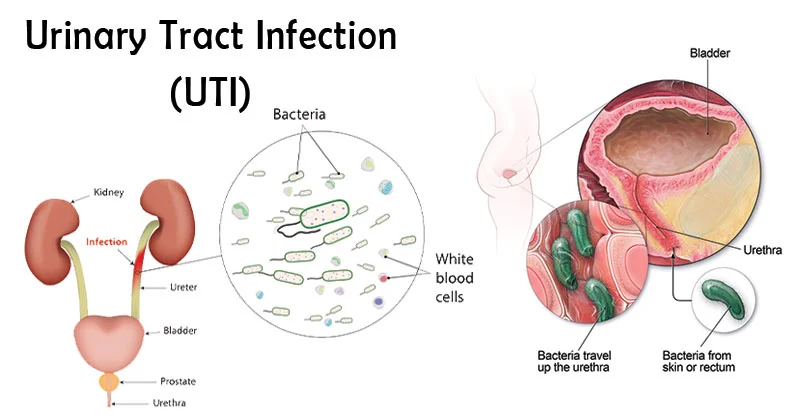
A complicated UTI is defined as an infection of the urinary tract that occurs in the presence of an underlying condition that complicates treatment, such as anatomical abnormalities, foreign devices like catheters, or a compromised immune system. Citrobacter is a genus of bacteria that, though commonly found in the gastrointestinal tract, can also cause infections in various body systems, including the urinary tract. When these bacteria are responsible for a UTI, it becomes classified as Citrobacter complicated UTI, often resulting in more severe symptoms and outcomes compared to uncomplicated infections.
Symptoms of Citrobacter Complicated UTI
Recognizing the symptoms of a complicated UTI is crucial for timely intervention and preventing the infection from escalating. Symptoms may include:
- Painful urination (dysuria): A burning sensation while urinating.
- Frequent urination: The urge to urinate more often than usual, even with little output.
- Urgency: A sudden, strong urge to urinate.
- Cloudy or foul-smelling urine: Often indicative of a bacterial infection.
- Lower abdominal or pelvic pain: Pain in the lower abdomen or pelvic region, especially when urinating.
- Fever and chills: Indicative of a more severe infection that may have spread to the kidneys (pyelonephritis).
- Nausea and vomiting: Common signs when the infection affects the kidneys.
- Fatigue and malaise: General feeling of illness and lack of energy.
Patients with underlying conditions like diabetes, kidney disease, or catheter use are at higher risk for developing complicated UTIs.
Causes of Citrobacter Complicated UTI
The primary cause of a Citrobacter complicated UTI is the invasion of Citrobacter species, which are part of the Enterobacteriaceae family. These bacteria can enter the urinary tract through several mechanisms:
- Ascending infection: The most common route, where bacteria ascend from the urethra to the bladder, kidneys, or other parts of the urinary system.
- Catheter-associated UTI: Patients with urinary catheters are at increased risk of infection due to the introduction of bacteria into the bladder.
- Anatomical abnormalities: Conditions such as kidney stones, structural deformities, or urinary retention may create environments conducive to bacterial growth.
- Weakened immune system: Conditions like diabetes, HIV, or immunosuppressive therapy make the body less capable of defending against bacterial invasions.
- Hospital-acquired infections: Citrobacter species are often found in healthcare settings, and prolonged hospital stays or surgical procedures may lead to infection.
Risk Factors for Developing Citrobacter Complicated UTI
Certain populations are more susceptible to developing a Citrobacter complicated UTI, including:
- Elderly individuals: Age-related changes in the immune system and urinary tract make older adults more vulnerable to infections.
- Women: Pregnancy, menopause, and certain contraceptive methods increase the risk of UTIs in women.
- Diabetic patients: High blood sugar levels can impair the immune system, making it harder to fight infections.
- People with urinary tract abnormalities: Conditions such as obstructive uropathy or congenital malformations increase the likelihood of infection.
- Immunocompromised individuals: Chemotherapy, organ transplants, and certain medications suppress the immune system, allowing bacteria to thrive.
Diagnosing Citrobacter Complicated UTI
Proper diagnosis of a Citrobacter complicated UTI is essential for effective treatment. The diagnostic process typically includes:
- Urinalysis: A routine test to detect signs of infection, such as white blood cells, bacteria, and blood in the urine.
- Urine culture: The gold standard for identifying the causative organism, in this case, Citrobacter. It also helps determine antibiotic susceptibility.
- Imaging tests: If a complicated infection is suspected, imaging tests like ultrasound or CT scans may be used to detect structural abnormalities in the urinary tract.
- Blood cultures: In cases where the infection may have spread to the bloodstream, blood cultures help identify the bacteria involved.
The presence of Citrobacter in urine cultures, along with clinical symptoms, confirms the diagnosis of a complicated UTI.
Treatment of Citrobacter Complicated UTI
The treatment of a Citrobacter complicated UTI typically involves both antibiotic therapy and management of any underlying conditions contributing to the infection.
1. Antibiotic Therapy
Antibiotics are the cornerstone of treatment. The choice of antibiotic will depend on the results of the urine culture and the susceptibility of the Citrobacter species. Common antibiotics used to treat Citrobacter infections include:
- Fluoroquinolones (e.g., ciprofloxacin)
- Third-generation cephalosporins (e.g., ceftriaxone)
- Carbapenems (e.g., meropenem) in severe cases
In severe or hospital-acquired cases, intravenous antibiotics may be required.
2. Addressing Underlying Conditions
Managing any underlying conditions, such as removing a catheter, draining an abscess, or treating a structural abnormality, is critical to prevent recurrent infections.
3. Supportive Care
In some cases, patients may require supportive care, including:
- Hydration: To help flush the bacteria from the urinary tract.
- Pain management: To alleviate discomfort associated with the infection.
4. Surgical Intervention
In rare cases, surgical procedures may be necessary to treat complications such as kidney abscesses or obstructed urine flow.
Prevention of Citrobacter Complicated UTI
Preventing Citrobacter complicated UTIs involves several key strategies:
- Proper hygiene: Cleanliness, especially around the genital and perineal area, is essential to prevent bacterial introduction.
- Adequate hydration: Drinking plenty of fluids helps flush the urinary tract, reducing the risk of infection.
- Proper catheter care: For those who require urinary catheters, appropriate care and timely replacement are essential to reduce infection risk.
- Management of underlying conditions: Keeping chronic conditions such as diabetes under control helps reduce the likelihood of infection.
- Antibiotic stewardship: The careful use of antibiotics is critical to prevent antibiotic resistance, especially in healthcare settings.